

BREAST CANCER CASE STUDY
Oct 01, 2014
960 likes | 5.69k Views
BREAST CANCER CASE STUDY. FRAZER BELL STUDENT BMS BSc APPLIED BIOMEDICAL SCIENCE. PATIENT HISTORY. 70 YEAR OLD FEMALE PRESENTED AT GP SURGERY 02/OCT/2012 EXAMINATION: RIGHT NIPPLE DRAWING IN & FIRM PALPABLE LUMP REFERRED TO THE BREAST CLINIC. BREAST CLINIC. ATTENDED 18/OCT/2012
Share Presentation
- receptor status
- oestrogen receptor
- staging investigations
- oestrogen receptor status
- sentinel lymph node biopsy

Presentation Transcript
BREAST CANCERCASE STUDY FRAZER BELL STUDENT BMS BSc APPLIED BIOMEDICAL SCIENCE
PATIENT HISTORY • 70 YEAR OLD FEMALE • PRESENTED AT GP SURGERY 02/OCT/2012 • EXAMINATION: RIGHT NIPPLE DRAWING IN & FIRM PALPABLE LUMP • REFERRED TO THE BREAST CLINIC
BREAST CLINIC • ATTENDED 18/OCT/2012 • EXAMINATION: INVERTED NIPPLE RETRACTION AND PALPABLE LUMP • ? PALPABLE LUMP RIGHT AXILLA • GRADED P5: MALIGNANT • FURTHER INVESTIGATIONS: MAMMOGRAM, ULTRASOUND & BREAST CORE BIOPSY
MAMMOGRAPHY • AREA OF SUSPICIOUS ABNORMALITY ON RIGHT BREAST • GRADED M4: PROBABLY MALIGNANT
ULTRASOUND • ULTRASOUND : CORRESPONDING 2CM AREA • GRADED U4: PROBABLY MALIGNANT
BIOPSY • ULTRASOUND GUIDED BREAST CORE BIOPSIES FROM THE RIGHT BREAST • ONE 13MM FIBROFATTY CORE PLUS 4 FIBROFATTY FRAGMENTS
NORMAL BREAST TISSUE
PATHOLOGY GRADED: B5b Infiltrating Breast Carcinoma
IMMUNOCYTOCHEMISTRY E-CAD NEGATIVE
RECEPTOR STATUS • OESTROGEN RECEPTOR & HER-2 STATUS • DETERMINE RECEPTOR STATUS FOR HORMONE THERAPY
OESTROGEN RECEPTOR STATUS NEGATIVE CONTROL OESTROGEN POSITIVE
PROGESTERONE REC. STATUS PROG POSITIVE NEGATIVE CONTROL
HER-2 STATUS HER2 NEGATIVE NEGATIVE CONTROL
TREATMENT PLAN • BREAST MDT MEETING • MASTECTOMY WITHOUT NEOADJUVANT TREATMENT • SENTINEL LYMPH NODE BIOPSY • SURGERY DATE 06/NOV/2012
PRE-OP ASSESSMENT • ADMITTED PRE-OP CLINIC 01/NOV/2012 • LABS TESTS: PRE-OP BLOODS • HYPERTENSIVE • MEDICAL WARD: ECG CONFIRMED LVH • SURGERY CANCELLED
TREATMENT PLAN • REDUCE BLOOD PRESSURE VIA ACE INHIBITORS • CHEST X-RAY & U/S OF KIDNEYS • STARTED ON LETROZOLE 2.5mg DAILY • BP MONITORED FORTNIGHTLY • RE-ASSESSMENT FOR SURGERY IN JANUARY
SURGERY • BP STABILISED • ADMITTED TO SURGICAL WARD 13/FEB/13 • SURGERY 25/FEB/13 • RIGHT BREAST MASTECTOMY • SENTINEL LYMPH NODE BIOPSY
MASTECTOMY • 19MM AND 7MM FIRM NODULES UPON DISSECTION • NO LYMPHOVASCULAR INVASION • 12MM CLEARANCE DEEP MARGIN
HISTOPATHOLOGY TUMOUR GRADE 2 INVASIVE LOBULAR CARCINOMA
SENTINEL LYMPH NODE • FIVE SENTINEL NODES • FOUR NEGATIVE • ONE POSITIVE DEPOSIT OF METASTATIC TUMOUR • ICC: AE1/AE3 CYTOKERATIN
SENTINEL LYMPH NODE AE1/AE3 POSITIVE H&E SENTINEL NODE
POST-OPERATIVE • GRADE 2 INVASIVE LOBULAR CARCINOMA • CLOSEST RELEVANT MARGIN 12MM • SINGLE NODE POSITIVITY • STAGING INVESTIGATIONS REQUIRED
STAGING INVESTIGATIONS • STAGING INVESTIGATIONS TO EXCLUDE METASTASES • CT SCAN - NEGATIVE • BONE SCAN - NEGATIVE
FUTURE • PATIENT DECLINED CHEMOTHERAPY • WILL ATTEND THE BEATSON CANCER CENTRE • RADIOTHERAPY TREATMENT • CONTINUE LETROZOLE
ACKNOWLEDGEMENTS • CONS. PATHOLOGIST Dr. A. W. Milne • CROSSHOUSE PATHOLOGY DEPT.
- More by User
BREAST CANCER STUDY
BREAST CANCER STUDY A STUDY OF ISSUES INVOLVING THE DIAGNOSIS OF BREAST CANCER THAT RESULT IN MEDICAL MALPRACTICE CLAIMS 2002 Breast Cancer Study Focus 450 cases involving paid claims with resolution dates no earlier than January 1, 1995 were analyzed.
769 views • 32 slides
Breast Cancer
Breast Cancer Casey and Tabitha What is it? Breast cancer is a cancerous tumor that starts from cells of the breast. The disease occurs mostly in women, but men can get breast cancer too. About 178,480 women in the United States will be found to have invasive breast cancer in 2007.
1.24k views • 9 slides
Breast Cancer. Locally Advanced and Metastatic Disease C. Legler MD FRCPC September 30, 2005. Locally Advanced and Metastatic Breast Cancer. Overview: Principles of neoadjuvant chemotherapy for locally advanced and inflammatory breast cancer Systemic therapy of metastatic breast cancer
2.03k views • 53 slides
Cervical Cancer Case Study
Cervical Cancer Case Study. Presented by: University of Guelph. Baktiar Hasan Mark Kane Melanie Laframboise Michael Maschio Andy Quigley. Objectives. To determine an appropriate model for the prediction of recurrence of cervical cancer
1.54k views • 22 slides

Breast Cancer. April 1, 2014. Introduction. Most common female cancer Accounts for 32% of all female cancer 211,300 new cases yearly and rising 40,000 deaths yearly. Gross Anatomy. Sappy’s plexus – lymphatics under areolar complex 75% of lymphatics flow to axilla. Microscopic Anatomy.
2.34k views • 33 slides
Cervical Cancer Case Study. Supervising Professor: Dr. P.D.M. Macdonald Team Members: Christine Calzonetti, Simo Goshev, Rongfang Gu, Shahidul Mohammad Islam, Amanda Lafontaine, Marcus Loreti, Maria Porco, William Volterman, Qihao Xie.
1.65k views • 17 slides
2002 Breast Cancer Study Focus . 450 cases involving paid claims with resolution dates no earlier than January 1, 1995 were analyzed.The study addresses only claims alleging a delay in the diagnosis of breast cancer.25 PIAA member companies reported information.. More than 68% of the patients repr
488 views • 32 slides

Breast Cancer. By George Rezk. What is Breast Cancer?. Breast cancer is a cancer that starts in the tissues of the breast. There are two main types of breast cancer :
758 views • 13 slides

Breast Cancer . By: Kalyn Johnson. So….What is breast cancer anyways???.
262 views • 7 slides

Breast Cancer. The Penncrest High School Medical Scholars Club. Things You probably don’t Know About Breast Cancer. -The older a woman, the more likely she is to get breast cancer -Young women can get breast cancer, even in their 20s
1.1k views • 41 slides
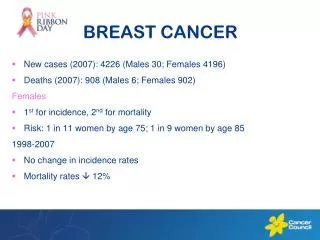

BREAST CANCER
BREAST CANCER. New cases (2007): 4226 (Males 30; Females 4196) Deaths (2007): 908 (Males 6; Females 902) Females 1 st for incidence, 2 nd for mortality Risk: 1 in 11 women by age 75; 1 in 9 women by age 85 1998-2007 No change in incidence rates Mortality rates 12%. BREAST CANCER.
1.27k views • 8 slides

Breast Cancer. The Penncrest High School Medical Scholars Club. 5 Things You probably don’t Know About Breast Cancer. -The older a woman, the more likely she is to get breast cancer -Young women can get breast cancer, even in their 20s
2.08k views • 51 slides
Carolina Breast Cancer Study: Breast cancer subtypes and race
Carolina Breast Cancer Study: Breast cancer subtypes and race. Robert Millikan University of North Carolina Chapel Hill, NC. Research Questions. Could breast cancer represent more than one disease? Can different subtypes of breast cancer help to explain racial disparities?.
806 views • 37 slides

Breast Cancer. By Shelby Palmer && Whitney Brosious. Sometimes, precancerous cells may be found within breast tissue. Regular healthy cells get mutated into cancer cells. They divide uncontrollably and quickly create many more or the same harmful cells.
589 views • 15 slides
Breast Cancer. Kathrina Calulut Alison Saechao. Breast Cancer. Cancer of tissues of the breast Ductal carcinoma Lobular carcinoma. Risk Factors. 1 in 8 women Age and Gender Family History Substance Abuse Childbirth Obesity. Early Symptoms. New lump or mass
808 views • 15 slides
Breast Cancer . Who Gets What Type of Surgery? Murray Pfeifer 16 th August, 2014. History of Breast Cancer Treatment. Hipppocrates (460-375BC) spoke of two cases Galen (129-200AD) Humoral theory Linked to melancholia Likened to a ‘crab’
1.42k views • 38 slides
Breast Cancer. An opportunity to save Lives. Behram Pastakia Metropolitan Washington DC USA 9 th World Zoroastrian Congress, Dubai 2009. Defining the Problem. Breast cancer strikes 1 in 8 women in their lifetime Family history can increase your risk
550 views • 24 slides
Case Study 63: Cancer of the Female Breast
Case Study 63: Cancer of the Female Breast. By Robyn Schwartz. Case Background. 46, premenopausal Dense breasts Has noticed cysts in the past Noticed new lump in upper right quadrant Did not resolve Got bigger Denied lumps in axillary. Patient history. Happily married for 21 years
1.57k views • 16 slides
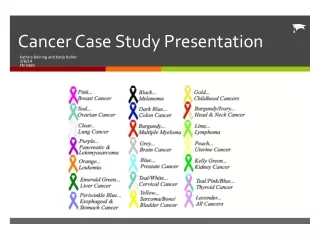
Cancer Case Study Presentation
Cancer Case Study Presentation. Katrina Beining and Katie Koller 2/8/14 FN 4360. What is Cancer?. Over 100 diseases 1 Cancer can cause almost any sign or symptom depending on size/location of tumor & how it effects organs and tissues 1. Etiology. In general 1 :
308 views • 14 slides
Case Study: Radiation Therapy and Ultrasound Management of Breast Cancer
Case Study: Radiation Therapy and Ultrasound Management of Breast Cancer. hhholdorf. Radiation Therapy (also known as radiotherapy and radiation oncology) began shortly after the discovery of X-rays in 1895 by Wilhelm Rontgen.
254 views • 22 slides
Breast cancer study group
Breast cancer study group. Outline. Adjuvant endocrine therapy Systemic disease Local disease Metastatic disease. Rationale for endocrine therapy of breast cancer. Estrogen and/or progesterone receptor expression is found in 85% of breast cancers. This proportion increases with age.
867 views • 79 slides

IMAGES
VIDEO
COMMENTS
This case study describes a 37-year-old female patient who presented with a breast mass. Diagnostic tests performed included a mammogram, biopsy, and right modified radical mastectomy which revealed invasive ductal carcinoma.
This case study summarizes a 38-year old female patient presenting with breast pain, nipple tenderness, and bloody discharge. Her medical history includes a diagnosis of tennis elbow. Laboratory tests and cytology reports were conducted.
This case study describes a 72-year-old retired female teacher who presented with a lump in her right breast and was diagnosed with invasive lobular carcinoma. She had a previous history of left breast cancer in 1986 and family history of various cancers.
Breast cancer is a cancer that starts in the cells of the breast in women and men . Worldwide, breast cancer is the second most common type of cancer after lung cancer, and the fifth most common cause of cancer death.
Breast Cancer : Overview of symptoms, causes, diagnosis, risk factor and treatment. Breast cancer is a disorder in women, which starts in the inner lining of milk ducts or the lobules that supply them milk. Breast cancer may include lump in the breast, a change in breast or red scaly patch on skin.
Case Study: Radiation Therapy and Ultrasound Management of Breast Cancer hhholdorf. Radiation Therapy (also known as radiotherapy and radiation oncology) began shortly after the discovery of X-rays in 1895 by Wilhelm Rontgen.