- Bibliography
- More Referencing guides Blog Automated transliteration Relevant bibliographies by topics
- Automated transliteration
- Relevant bibliographies by topics
- Referencing guides

Dissertations / Theses on the topic 'Training in midwifery'
Create a spot-on reference in apa, mla, chicago, harvard, and other styles.
Consult the top 17 dissertations / theses for your research on the topic 'Training in midwifery.'
Next to every source in the list of references, there is an 'Add to bibliography' button. Press on it, and we will generate automatically the bibliographic reference to the chosen work in the citation style you need: APA, MLA, Harvard, Chicago, Vancouver, etc.
You can also download the full text of the academic publication as pdf and read online its abstract whenever available in the metadata.
Browse dissertations / theses on a wide variety of disciplines and organise your bibliography correctly.
Phiri, Wendy Augusta. "Perceptions and experiences of undergraduate midwifery students concerning their midwifery training." Thesis, Stellenbosch : University of Stellenbosch, 2011. http://hdl.handle.net/10019.1/6659.
Pama, Nomzekelo. "Factors affecting experiential learning for midwifery students at the public college of nursing in the Eastern Cape." Thesis, University of Fort Hare, 2017. http://hdl.handle.net/10353/4524.
Sage-Pranchère, Nathalie. "L’école des sages-femmes. Les enjeux sociaux de la formation obstétricale en France, 1786-1916." Thesis, Paris 4, 2011. http://www.theses.fr/2011PA040258.
Alhassan, Mustapha [Verfasser], Stefan [Gutachter] Wilm, and Andrea [Gutachter] Icks. "Communication skills training (CST) to enhance nursing and midwifery students’ empathy, communicative competence, communication skills attitude, and self-efficacy / Mustapha Alhassan. Gutachter: Stefan Wilm ; Andrea Icks." Düsseldorf : Universitäts- und Landesbibliothek der Heinrich-Heine-Universität Düsseldorf, 2016. http://d-nb.info/1104367041/34.
Bouchot, Hélène. "Observer autrui lors de séances de simulation haute-fidélité : une activité mimétique et ludique portée par des en-jeux sérieux." Thesis, Montpellier, 2019. http://www.theses.fr/2019MONTS104.
Laniel, Valérie. "Apprentissage par simulation et activité du formateur : comment le travail avec un simulateur d'accouchement interactif a-t-il développé l'activité d'une enseignante en maïeutique?" Thesis, Montpellier 3, 2015. http://www.theses.fr/2015MON30063/document.
Balogh, Ruth P. "Performance monitoring for nurse & midwife training institutions : some problems for the conduct of action research." Thesis, Institute of Education (University of London), 1993. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.252002.
Balogh, Ruth Penelope. "Using action research to develop a national performance monitoring framework for nurse and midwife training institutions." Thesis, University College London (University of London), 1993. http://discovery.ucl.ac.uk/10018907/.
Meyer, Rushaan. "The experiences of male nurses in midwifery clinical training at a regional hospital in the Eastern Cape." Diss., 2012. http://hdl.handle.net/10500/10572.
Mthombeni, Courage Salvah. "A model to enhance training for male student nurses in midwifery nursing science in the Limpopo Province." Thesis, 2018. http://hdl.handle.net/11602/971.
Malwela, Thivhulawi. "Integration of midwifery nursing science theory with clinical practice in selected training hospitals of Vhembe District, Limpopo Province." Diss., 2015. http://hdl.handle.net/11602/249.
Setumo, Lefoka Johanna. "Midwifery students' experiences of clinical teaching at Sovenga Campus (Limpopo College of Nursing), Limpopo province." Diss., 2013. http://hdl.handle.net/10500/14362.
"A continuing professional development system for nurses and midwives in South Africa." Thesis, 2008. http://hdl.handle.net/10210/1719.
CHUNG, MENG-CHIN, and 鍾孟津. "Midwife Training System and Practice in Japan-Ruled Taiwan: Chen, He's Notes of Midwife Trainings." Thesis, 2016. http://ndltd.ncl.edu.tw/handle/h74df8.
Chen, Hui-Hsuan, and 陳慧軒. "“Midwife or dukun bayi?” : the midwife training system in Dutch East Indies, c. 1850-1915." Thesis, 2012. http://ndltd.ncl.edu.tw/handle/47544399515420494754.
Sikhitha, Rathani Mabel. "The development of nursing and nursing education in Venda from 1911 to 1990." Diss., 1997. http://hdl.handle.net/10500/16034.
Bedon, Peggy S. M. "Pratiques traditionnelles chez les sages-femmes autochtones du Nunavik et programme de formation." Thèse, 2008. http://hdl.handle.net/1866/2902.
- How it works
"Christmas Offer"
Terms & conditions.
As the Christmas season is upon us, we find ourselves reflecting on the past year and those who we have helped to shape their future. It’s been quite a year for us all! The end of the year brings no greater joy than the opportunity to express to you Christmas greetings and good wishes.
At this special time of year, Research Prospect brings joyful discount of 10% on all its services. May your Christmas and New Year be filled with joy.
We are looking back with appreciation for your loyalty and looking forward to moving into the New Year together.
"Claim this offer"
In unfamiliar and hard times, we have stuck by you. This Christmas, Research Prospect brings you all the joy with exciting discount of 10% on all its services.
Offer valid till 5-1-2024
We love being your partner in success. We know you have been working hard lately, take a break this holiday season to spend time with your loved ones while we make sure you succeed in your academics
Discount code: RP0996Y

Useful Links
How much will your dissertation cost?
Have an expert academic write your dissertation paper!
Dissertation Services
Get unlimited topic ideas and a dissertation plan for just £45.00
Order topics and plan
Get 1 free topic in your area of study with aim and justification
Yes I want the free topic
Midwifery Dissertation Topics
Published by Owen Ingram at January 3rd, 2023 , Revised On August 16, 2023
There have been midwives around for decades now. The role of midwives has not changed much with the advent of modern medicine, but their core function remains the same – to provide care and comfort to pregnant women during childbirth.
It is possible to be a midwife in the healthcare industry, but it is not always a rewarding or challenging career. Here are five things you didn’t know about midwifery nursing to help you decide if it could be the right career choice for you.
The profession of midwifery involves caring for women and newborns during pregnancy, childbirth, and the first few days following birth. Registered nurses are trained with four additional years of education along with major research on methods involve in midwifery and writing on midwifery dissertation topics, while midwives provide natural health care for mothers and children.
As a midwife, your role is to promote healthy pregnancies and births while respecting women’s rights and dignity. Midwives provide care to patients at every stage of life, from preconception to postpartum, family planning to home delivery to breastfeeding support.
Important Links: Child Health Nursing Dissertation Topics , Adult Nursing Topics , Critical Care Nursing Dissertation Topics . These links will help you to get a broad experience or knowledge about the latest trends and practices in academics.
Midwifery Is A Good Fit for the Following:
● Those who want to work with women, especially those at risk of giving birth in a hospital setting. ● Those who enjoy helping people and solving problems. ● Those who like to be creative and solve complex problems. ● Those who want to help others and make a difference in their lives.
Midwifery is a career with many benefits for both the midwife and the baby. They are well-trained and experienced in caring for pregnant women and newborns and often have access to the exceptional care that other nurses may not have.
Related Links:
- Evidence-based Practice Nursing Dissertation Topics
- Child Health Nursing Dissertation Topics
- Adult Nursing Dissertation Topics
- Critical Care Nursing Dissertation Topics
- Dementia Nursing Dissertation Topics
- Palliative Care Nursing Dissertation Topics
- Mental Health Nursing Dissertation Topics
- Nursing Dissertation Topics
- Coronavirus (COVID-19) Nursing Dissertation Topics
Midwifery Dissertation Topics With Research Aim
Topic:1 adolescence care.
Research Aim: Focus on comprehensive medical, psychological, physical, and mental health assessments to provide a better quality of care to patients.
Topic:2 Alcohol Abuse
Reseasrch Aim: Closely studying different addictions and their treatments to break the habit of drug consumption among individuals.
Topic:3 Birth Planning
Research Aim: Comprehensive birth planning between parents discussing the possible consequences of before, between, and after labour.
Topic:4 Community midwifery
Research Aim: Studying different characters in community midwifery and the midwife’s role in providing care for the infant during the early days of the child’s birth.
Topic:5 Contraception
Research Aim: Understand the simplicity of contraception to prevent pregnancy by stopping egg production that results in the fertilization of egg and sperm in the later stages.
Topic:6 Electronic fetal monitoring
Research Aim: In-depth study of electronic fetal monitoring to track the health of your baby during the womb, record construction per minute, and make a count of your baby’s heart rate.
Topic:7 Family planning
Research Aim: Importance to follow the basic rhythm methods for the couple to prevent pregnancy and use protection during the vaginal sex to plan a family without fertility treatments.
Topic:8 Foetal and newborn care
Research Aim: Expansion of the maternal-fetal and newborn care services to improve the nutritional quality of infants after delivery during their postnatal care time.
Topic:9 Foetal well being
Carefully tracking indications for the rise in heart rate of the fetal by weekly checkups to assess the overall well-being of the fetal.

Topic:10 Gender-based violence
Research Aim: Studying the consequences of male desire for a child that results in gender-based violence, harming the child’s physical and mental health.
Topic:11 Health promotion
Research Aim: Working on practices that help in controlling the amount of pollution of people, taking care of their overall health, and improving quality of life through adapting best health practices.
Topic:12 High-risk pregnancy
Research Aim: Calculating the ordinary risks of a high-risk pregnancy and how it affects a pregnant body resulting in a baby with poor health or any by-birth diseases, increasing the chance for complications.
Topic:13 HIV infection
Research Aim: Common causes of HIV infection and their long-term consequences on the body’s immune system. An in-depth study into the acquired immunodeficiency and the results leading to this.
Topic:14 Human Rights
Creating reports on human rights and their link with the freedom of thought, conscience, religion, belief, and other factors.
Topic:15 Infection prevention and control
Research Aim: Practices for infection prevention and control using efficient approaches for patients and health workers to avoid harmful substances in the environment.
Topic:16 Infertility and pregnancy
Research Aim: Evaluating the percentage of infertility and pregnancy, especially those facing no prior births, and who have high chances of infertility and pregnancy complications.
Hire an Expert Writer
Orders completed by our expert writers are
- Formally drafted in an academic style
- Free Amendments and 100% Plagiarism Free – or your money back!
- 100% Confidential and Timely Delivery!
- Free anti-plagiarism report
- Appreciated by thousands of clients. Check client reviews
I/O Example
Midwives are nurses who provide continuous support to the mother before, during, and after labour. Midwives also help with newborn care and educate parents on how to care for their children.
How Much Do Midwives Make?
The salary of a midwife varies depending on the type of work, location, and experience of the midwife. Midwives generally earn $132,950 per year. The average annual salary for entry-level midwives is $102,390.
The minimum requirement for becoming a midwifery nurse is a bachelor’s degree in nursing, with the option of pursuing a master’s degree.
An accredited educational exam can also lead to certification as a nurse-midwife (CNM). The American College of Nurse-Midwives (ACNM) enables you to practice independently as a midwife.
There are many pros and cons to working as a midwife. As a midwife, you have the following pros and cons:
- Midwives have the opportunity to help women during one of the most memorable moments in their lives.
- Midwives can positively impact the health of mothers and their children.
- Midwives can work in many hospitals, clinics, and homes.
- In midwifery, there are many opportunities for continuing education and professional development.
- You will often have to work nights and weekends, which can be mentally draining.
- You will have to travel a lot since most births occur in hospitals or centres in different areas.
- You will have to deal with stressors such as complex patients and uncooperative families.
- You will be dealing with a lot of pain, so you need to be able to handle it without medication or other treatment methods.
A career in midwifery is a great fit for those with a passion for health and wellness, an interest in helping people, and a desire to work in a supportive environment.
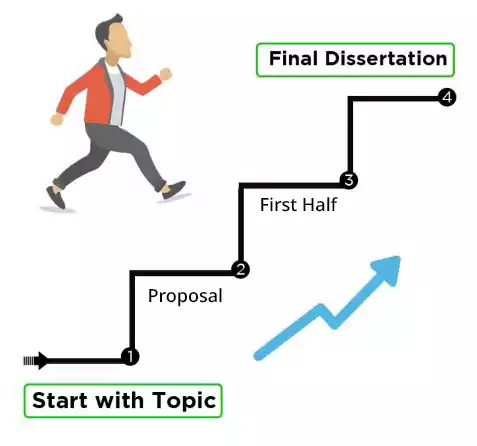
It is important to become involved in your local midwifery community if you are contemplating a career in midwifery – the best source of learning is your major research work, along with writing a lengthy thesis document on midwifery dissertation topics that will submit to your university to progress your midwifery career.
Free Dissertation Topic
Phone Number
Academic Level Select Academic Level Undergraduate Graduate PHD
Academic Subject
Area of Research
Frequently Asked Questions
How to find midwifery dissertation topics.
To find midwifery dissertation topics:
- Explore childbirth challenges or trends.
- Investigate maternal and infant health.
- Consider cultural or ethical aspects.
- Review recent research in midwifery.
- Focus on gaps in knowledge.
- Choose a topic that resonates with your passion and career goals.
You May Also Like
Property, land, buildings, air rights, underground rights, and underground rights are examples of real estate. Academics recognize the importance of real estate as a driver of the economy. This field will be encountered by college and university students studying business-related courses.
Here is a list of Research Topics on Art and culture, choose the one that suits your requirements.
In general, business law regulates the legal rights, conducts, and relationships of individuals with businesses engaged in trade, commerce, or other commercial activities. The subject covers a broad range of ideas that fall under the business law.
As Featured On

USEFUL LINKS
LEARNING RESOURCES

COMPANY DETAILS

Splash Sol LLC
- How It Works
