Using CPT modifiers effectively to ensure accurate coding and billing
CPT Modifiers List in medical billing and Coding
CPT modifiers are essential tools in medical coding and billing as they provide additional information to accurately define a procedure or service rendered by a healthcare provider. Proper use of modifiers is crucial to ensure accurate reimbursement, prevent claim denials, and maintain compliance with coding guidelines. In this article, we will explore tips and best practices for using CPT modifiers effectively:
1. Understand the Purpose of Modifiers:
It is crucial to have a clear understanding of the purpose of modifiers before applying them to a CPT code. They provide additional information to payers to explain the specific circumstances of a service.
2. Familiarize Yourself with Common Modifiers:
There are a multitude of CPT modifiers available, each serving a different purpose. It is important to familiarize yourself with the most commonly used modifiers such as 59 (distinct procedural service), 25 (significant, separately identifiable evaluation and management service), and 51 (multiple procedures).
3. Review Payer Policies:
Different payers may have specific guidelines and policies regarding the use of modifiers. It is important to review payer-specific rules to ensure compliance and prevent rejections or denials of claims. Understanding the requirements of different payers can help you apply modifiers appropriately.
4. Use Modifiers to Avoid Denials:
One of the main purposes of modifiers is to prevent claim denials. By using modifiers appropriately to indicate different circumstances or services provided, you can ensure that the claim is processed correctly and reimbursed in a timely manner.
5. Avoid Unbundling:
One common error in coding is unbundling, where separate procedures are billed individually instead of using the appropriate bundled code with a modifier. This can lead to claim denials and accusations of fraudulent billing. Be sure to use modifiers like 59 to clearly indicate separate procedures when necessary.
6. Document Clinical Justification:
When using modifiers such as 25 for a separately identifiable E/M service, it is essential to ensure that the medical record supports the need for the additional service. Proper documentation is key to justifying the use of modifiers and ensuring accurate coding and billing.
7. Use Modifiers Ethically:
Maintaining ethical standards in medical coding and billing is crucial. Avoid using modifiers inappropriately to increase reimbursement or deceive payers. Adhering to professional ethics and coding guidelines is essential for ensuring accurate and compliant billing practices.
8. Stay Updated with Coding Changes:
It is important to stay updated with coding changes and modifications to ensure accurate coding and billing practices. Keeping abreast of industry updates and attending continuing education programs can help you stay informed and proficient in using CPT modifiers effectively.
9. Communicate with Providers:
Clear communication between coders and healthcare providers is essential for accurate coding and billing. Providers should document services accurately to support the use of modifiers, and coders should communicate any discrepancies or missing information to ensure proper reimbursement and compliance.
10. Conduct Regular Audits:
Performing regular audits of coding practices can help identify errors or inconsistencies in the use of modifiers. By conducting thorough reviews of coding processes and documentation, you can ensure compliance with coding guidelines and identify areas for improvement.
In conclusion, utilizing CPT modifiers effectively is essential for accurate coding and billing in healthcare. By understanding the purpose of modifiers, familiarizing yourself with common modifiers, reviewing payer policies, and following best practices outlined in this article, you can ensure proper reimbursement, prevent claim denials, and maintain compliance with coding guidelines. By incorporating these tips into your coding practices, you can enhance the accuracy and efficiency of your medical coding and billing processes.
- Understand the Importance, purpose and use of CPT modifiers in medical coding
- Impact: How CPT modifiers can affect reimbursement rates

Leave a Reply
Your email address will not be published. Required fields are marked *
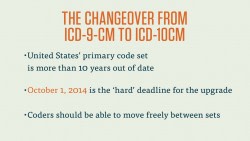
2.09: CPT Modifiers
When a simple CPT code isn’t enough, we turn to CPT modifiers. These important additions to CPT codes give extra information about how, where and why a procedure was performed. This video will introduce and explain CPT modifiers and how to use them.

Section 2.01
Learn More About Medical Coding

Section 2.02
Medical Coding Vocabulary & Key Terms
Section 2.05

Section 2.06
Using ICD-10-CM

Section 2.07
Intro to CPT Coding

Section 2.08
Section 2.09
CPT Modifiers
Section 2.10
Learn Medical Terminology and Human Anatomy
Section 2.11
HCPCS Codes
Section 2.12
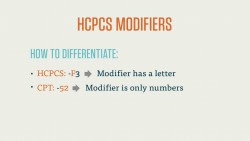
HCPCS Modifiers
Section 2.13
Crosswalking
Section 2.14
Electronic vs. Paper Coding

Section 2.15
Medical Coding Review
Since medical procedures and services are often complex, we sometimes need to supply additional information when we’re coding. CPT Modifiers , like modifiers in the English language, provide additional information about the procedure. In English, a modifier may describe the who, what, how, why, or where of a situation. Similarly, a CPT modifier may describe whether multiple procedures were performed, why that procedure was necessary, where the procedure was performed on the body, how many surgeons worked on the patient, and lots of other information that may be critical to a claim’s status with the insurance payer.
CPT Modifiers are always two characters, and may be numeric or alphanumeric. Most of the CPT modifiers you’ll see are numeric, but there are a few alphanumeric Anesthesia modifiers that we’ll look at toward the end of this course.
CPT modifiers are added to the end of a CPT code with a hyphen. In the case of more than one modifier, you code the “functional” modifier first, and the “informational” modifier second. The distinction between the two is simple: you always want to list the modifiers that most directly affect the reimbursement process first.
There’s a straightforward reason to this, too. While CMS-1500 and UB-04 forms, the two most common claim forms, have space for four modifiers, payers don’t always look at modifiers after the first two. Because of this, you always want the most important modifiers to be visible. We’ll return to this point in a few examples after we examine the CPT modifiers.
Bear in mind that each of the CPT modifiers you’ll find in this course are A) copyrighted by the American Medical Association (AMA) and B) contingent on a number of factors and guidelines. In other words, there are rules for their use. You can’t simply add a modifier to the end of a procedure code if you think it makes sense. There are, for example, a number of modifiers that state they are not compatible with Evaluation and Management (E&M) codes.
Let’s take a quick look at a an example of a CPT modifier in action.
A surgeon performs a procedure to remove a bone cyst in the upper arm of a patient. The procedure also includes obtaining a graft from elsewhere in the body. Due to minor complications, the surgeon is unable to fully excise the bone cyst.
For the procedure, we’d code 23140 for “excision or curretage of bone cyst or benign tumor, humerus; with autograft (includes obtaining the graft).” Since the procedure was completed but not fully successful, we’d add the -52 modifier, for reduced services, to the code, and we’d end up with 23140-52.
Physical Status Modifier (for Anesthesia)
Anesthesia procedures have their own special set of modifiers, which are simple and correspond to the condition of the patient as the anesthesia is administered. These codes are:
- P1 – a normal, healthy patient
- P2 – a patient with mild systemic disease
- P3 – a patient with severe systemic disease
- P4 – a patient with severe systemic disease that is a constant threat to life
- P5 – a moribund patient who is not expected to survive without the operation
- P6 – a declared brain-dead patient whose organs are being removed for donor purposes
As we said, these are relatively straightforward, but let’s look at an example that will also use some of the CPT modifiers we learned just a minute ago.
Let’s return to that angioplasty example. The patient needs to be anesthetized before undergoing this procedure, so we turn to the Anesthesia section of the CPT codebook and find the code 00216 for “vascular procedures.” Now, kidney problems notwithstanding, our patient is in good health, so we’d add the –P1 modifier to this anesthesia code, and end up with 00216-P1.
Modifiers Approved for Ambulatory Surgery Center (ASC) Hospital Outpatient Use
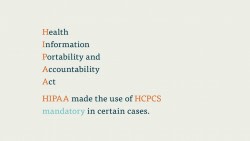
CPT modifiers are also used in ambulatory surgery centers (ASC). These hospital outpatient facilities specialize in procedures where the patient leaves the same day. Note that there may be some overlap or contradiction with the set of HCPCS modifiers, which we’ll cover in more depth later on.
For example, HCPCS codes , which are used to report procedures to Medicare and Medicaid, have modifiers that describe which side of the body a procedure is performed on.
We won’t dive much deeper than that for now, but just know that HCPCS, another important code set that shares a lot with CPT, has its own set of modifiers, and that it’s important to note which format you need to use for a particular claim.
Supplemental Reports
Many CPT modifiers require supplemental reports to the health insurance payer. If, for instance, a payer wants to know why a surgery to repair lesions on the liver of a patient was discontinued (let’s say there was a complication with one of the proximal organs), the coder would want to file a supplementary report stating this. We both want to code to the highest level of specificity and provide as much documentation as possible. If a modifier that requires justification of medical necessity is left without a supplemental report, the claim that procedure is on may very well be rejected.
Video: Cross Procedural Terminology (CPT) Modifiers
Unlock a career in medical billing and coding and make a difference in the healthcare industry.
Discover schools with specialized programs that empower you to make a difference today.


List Of All CPT Modifiers (2023) | Descriptions & Modifier Explanation
Below, you can find a list of all the CPT modifiers. A modifier ‘modifies’ a procedure or item and adds information or changes a description based on the documentation provided by the physician. First, we’ll explain what modifiers are before providing the CPT modifiers list.
CPT modifiers are added to CPT or HCPCS codes to provide additional information to the claim for the insurance payer and aim to clarify the procedure.
For example, additional information is required if a provider performed multiple procedures, if the medical necessity of a procedure needs to be explained, or if a procedure was performed on the right or left side of the body.
The CPT modifiers have two numeric digits, are copyrighted by the American Medical Association, and are updated annually.
The following examples from the CPT book explain appropriate scenarios for appending CPT modifiers to a claim:
- For procedures provided more than once (to the same patient).
- For billing bilateral (two-sided) procedure(s).
- For reduced or increased procedures
- For procedures performed in more than one location.
- For procedures provided by more than one provider.
- For professional and technical components.
Simply put, CPT modifiers add information to a CPT code about why, where, and how the procedure was performed.
TIP: Are you looking for a list with the HCPCS modifiers instead of the CPT modifiers? You can find the complete list of HCPCS modifiers here.
The CPT modifiers are divided into three categories. The first category of modifiers ranges from 22 to 99 and is called ‘Provider Services and Ambulatory Service Center Modifiers.’
The second category of CPT modifiers is also known as ‘performance measure modifiers’ or ‘ category II modifiers.’ They may be used to indicate that a procedure was considered but not performed due to;
- medical reasons;
- patient reasons;
- system reasons; or
- system circumstances.
The third category of CPT modifiers may be used to describe anesthesia services, known as ‘anesthesia physical status’ modifiers.

1. Modifier 21 (Deleted)
This modifier was deleted on 01-01-2009 and was used for prolonged evaluation and management services. Instead, you can use CPT 99354 , CPT 99355, CPT 99356, CPT 99357, CPT 99358 , or CPT 99359.
Learn more about the 21 modifier.
2. Modifier 22
Use this modifier for increased procedural services. The circumstances of the surgery need to be unusual and require more mental and/or physical work from the surgeon than usual.
Learn more about the 22 modifier.
3. Modifier 23
This modifier may be used in procedures with unusual anesthesia. Append this modifier when the provider uses anesthesia for a procedure that usually doesn’t require it.
Learn more about the 23 modifier.
4. Modifier 24
Append this modifier to an E/M service if a provider performed it during the global surgery period. The E/M must be unrelated to the patient’s surgery.
Learn more about the 24 modifier.
5. Modifier 25
This modifier may be used when a provider performs an E/M service on a patient on the same day as another procedure or service.
Learn more about the 25 modifier.
6. Modifier 26
This modifier identifies the professional component of a service and shows that a physician provides the interpretation and supervision of a procedure.
Learn more about the 26 modifier.
7. Modifier 27
Append this modifier to a subsequent, separate, and distinct E/M service for patients who received multiple E/M services with different providers on the same day and in the same hospital.
Learn more about the 27 modifier.
8. Modifier 32
This modifier can be appended for mandated services. Third parties, such as a legislative, governmental, or regulatory requirement, mandate that a provider performs a service.
Learn more about the 32 modifier.
9. Modifier 33
Append this modifier for preventive services. The primary function of a preventive service is to screen for specific diseases. Do not append this modifier to services with the word ‘screening’ in the description (for example, screening mammogram ).
Learn more about the 33 modifier.
10. Modifier 47
Append this modifier to a service or procedure when the performing surgeon also administered general or local anesthesia.
Learn more about the 47 modifier.
11. Modifier 50
This modifier may be used for bilateral radiology, diagnostic, or surgical procedures. A bilateral procedure is performed on both sides of the patient’s body during the same session.
Learn more about the 50 modifier.
12. Modifier 51
Append this modifier to multiple subsequent procedures if performed by the same provider, on the same patient, and during the same encounter.
Learn more about the 51 modifier.
13. Modifier 52
Append this modifier to reduced services. Use this modifier if a provider did not completely perform the procedure described by the code descriptor.
Learn more about the 52 modifier.
14. Modifier 53
Use this modifier for discontinued procedures. Report this modifier if a surgical or diagnostic procedure is terminated because it threatens the patient’s health.
Learn more about the 53 modifier.
15. Modifier 54
Report this modifier when a provider performs a procedure but does not provide postoperative or preoperative management.
Learn more about the 54 modifier.
16. Modifier 55
This modifier may be used when a provider performs postoperative management but they do not provide intraoperative or preoperative services.
Learn more about the 55 modifier.
17. Modifier 56
This modifier can be appended to a procedure if a provider performs preoperative management only and does not provide postoperative or intraoperative services.
Learn more about the 56 modifier.
18. Modifier 57
Append this modifier to a code if a provider decides to perform the surgery on the day or the day before the E/M service.
Learn more about the 57 modifier.
19. Modifier 58
This modifier may be appended to procedures performed during the postoperative period when a procedure is staged or planned.
Learn more about the 58 modifier.
20. Modifier 59
This is one of the common modifiers and identifies a distinct or independent procedural service from other non–E/M services performed on the same day by the same provider.
Learn more about the 59 modifier.
21. Modifier 62
Append this modifier for procedures performed by two primary surgeons, performing a distinct part of the procedure.
Learn more about the 62 modifier.
22. Modifier 63
This modifier can be appended to procedures performed on infants weighing less than four kilograms.
Learn more about the 63 modifier.
23. Modifier 66
Use this modifier when the provider who performed it was part of a surgical team because the procedure was difficult or highly complex.
Learn more about the 66 modifier.
24. Modifier 73
Append this modifier for discontinued ambulatory surgery centers or outpatient hospital procedures terminated before anesthesia was provided to the patient.
Learn more about the 73 modifier.
25. Modifier 74
This modifier can be used for discontinued ambulatory surgery centers or outpatient hospital-terminated procedures after the administration of anesthesia.
Learn more about the 74 modifier.
26. Modifier 76
You can use this modifier if the same provider repeats a procedure after they performed the initial procedure.
Learn more about the 76 modifier.
27. Modifier 77
Append this modifier to a code if a different provider repeats a procedure because the initial same procedure was not successful and was performed by another provider.
Learn more about the 77 modifier.
28. Modifier 78
Use this modifier when you bill a procedure provided by the same provider but unrelated to the initial procedure and performed during the postoperative period.
Learn more about the 78 modifier.
29. Modifier 79
Append this modifier if an unrelated procedure is performed during the postoperative period, the original procedure by the same provider.
Learn more about the 79 modifier.
30. Modifier 80
This modifier indicates that an assistant surgeon was present during the procedure and assisted a principal or operating surgeon.
Learn more about the 80 modifier.
31. Modifier 81
Append this modifier if an assistant surgeon was present during a part of the procedure and assisted a principal or operating surgeon.
Learn more about the 81 modifier.
32. Modifier 82
Use this modifier if an assistant surgeon was present during the entire procedure and assisted the operating or principal surgeon because a medical resident was unavailable.
Learn more about the 82 modifier.
33. Modifier 90
This modifier can be used when an outside or reference laboratory performs a pathology or laboratory test instead of the reporting or treating provider.
Learn more about the 90 modifier.
34. Modifier 91
You can use this modifier for repeated lab tests for the same patient and on the same day.
Learn more about the 91 modifier.
35. Modifier 92
This modifier identifies a disposable, single-use, transportable lab test or kit with an analytical chamber.
Learn more about the 92 modifier.
36. Modifier 93
Use this modifier for audio–only technology services that allow synchronous real-time interaction between patient and provider.
Learn more about the 93 modifier.
37. Modifier 95
Append this modifier for synchronous or real–time audiovisual conference services that allow the provider to provide healthcare from a different location than the patient.
Learn more about the 95 modifier.
38. Modifier 96
Habilitative services can be identified with this modifier. These services improve, maintain, and develop their skills to perform instrumental activities of daily living (IADLs) or activities of daily living (ADLs).
Read more about the 96 modifier.
39. Modifier 97
Rehabilitative services are indicated with this modifier. These services help patients restore or improve functions or skills lost due to disease or illness.
Read more about the 97 modifier.
40. Modifier 99
Report modifier 99 as the first modifier on a claim when the service or procedure requires more than one modifier.
Read more about the 99 modifier.

41. Modifier 1P
Use this modifier for a quality reporting code if a patient’s medical status prevents the provider from action.
42. Modifier 2P
This modifier indicates that a provider couldn’t act for patient reasons, such as refusal.
43. Modifier 3P
This modifier indicates that the provider did not act due to the healthcare delivery system.
44. Modifier 8P
Report this modifier if a provider could not act but did not specify the reason for not providing the action for a patient.
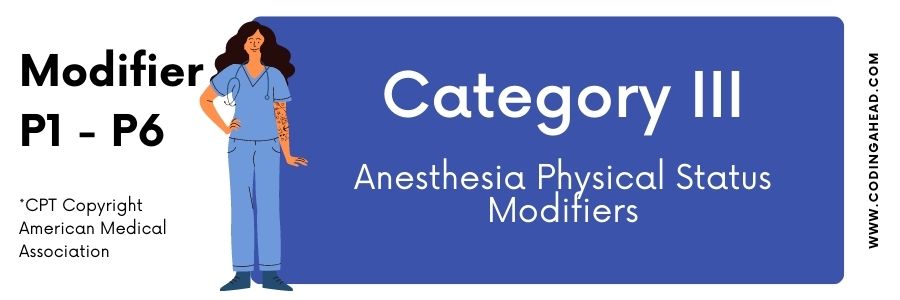
45. Modifier P1
Report this physical status modifier to identify anesthesia services provided by a physician to a normal and healthy patient.
46. Modifier P2
Report this physical status modifier to identify anesthesia services provided by a physician to a patient with mild systemic disease.
47. Modifier P3
Report this physical status modifier to identify anesthesia services provided by a physician to a patient with severe systemic disease.
48. Modifier P4
Report this physical status modifier to identify anesthesia services a physician provides to a patient suffering from a severe systemic disease that constantly threatens their life.
49. Modifier P5
Report this physical status modifier to identify anesthesia services provided by a physician to a dying patient who is not expected to survive without an operation.
50. Modifier P6
Report this physical status modifier to identify anesthesia services provided by a physician to a dead declared patient whose organs are removed to be donated.
Tip: You can find the HCPCS Level II Modifiers list here.
51. References
CPT Professional 2022
https://www.cms.gov/files/document/chapter1generalcorrectcodingpoliciesfinal11.pdf
Similar Posts

(2023) CPT 99391 – CPT 99397 | Established Patient Preventive Medicine Services
CPT 99391 & CPT 99392 Description: CPT 99391 & CPT 99392 can be used when a physician does a comprehensive review of past family and social history (PFSH), performs a comprehensive review of systems, and makes an assessment of gender-related risk factors and age. The physician may administer immunizations during the preventive service and obtain…
How To Use CPT Code 54015
CPT 54015 describes the procedure of incision and drainage of the penis, specifically for deep abscesses, cysts, or lesions. This article will cover the official description, procedure details, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 54015? CPT 54015 is used to describe the incision…
CPT Codes For Hydration Infusion
Below is a list summarizing the CPT codes for hydration infusion. CPT Code 96360 CPT 96360 describes the initial 31 minutes to 1 hour of intravenous infusion hydration. CPT Code 96361 CPT 96361 describes an add-on procedure for administering additional hours of intravenous hydration.
How To Use CPT Code 23620
CPT code 23620 describes the closed treatment of a greater humeral tuberosity fracture without manipulation. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 23620? CPT code 23620 is used to describe the closed treatment of a greater humeral…
How To Use CPT Code 57061
CPT 57061 describes the destruction of small or simple vaginal lesions using various methods such as laser surgery, electrosurgery, cryosurgery, or chemosurgery. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 57061? CPT 57061 can be used to describe…
How To Use CPT Code 67036
CPT 67036 describes a specific procedure performed on the posterior segment of the eye known as vitrectomy. This article will provide an overview of CPT code 67036, including its official description, the procedure itself, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 67036? CPT 67036…

- Medical Billing
- Credentialing
- Payer Contracting
- Behavioral Health
- Genetic Testing
- Pharmacogenetic (PGx) Testing
- COVID-19 Testing
- Allergy Testing
- Skilled Nursing Facilities
- Urgent Care
- Biologics and Specialty Drugs
- Telestroke and Teleneurology
- Remote Patient Monitoring
- Speech Therapy
- Home Infusion Therapy
- Substance Abuse
- Sleep Study Labs
- Physical Therapy (PT)
- Occupational Therapy
- HL7 Integration
Anatomic Modifiers
What are and when to use modifier codes.

What are Modifier Codes?
Modifier codes are two-digit codes appended to Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) codes . They indicate that the main procedure code has been altered in some way. Modifiers provide additional details about the service provided, which helps determine appropriate reimbursement.
Some key facts about modifier codes:
- Modifiers always follow the 5-digit CPT or HCPCS code they modify.
- There are two types of modifiers – CPT modifiers developed by the American Medical Association and HCPCS Level II modifiers developed by CMS .
- Over 340 modifier codes exist today.
- Modifiers help avoid incorrect or denied claims by specifying additional details.
- They should only be used when appropriate and necessary.
- Inappropriate use of modifiers can be considered fraudulent billing .
Simply put, modifiers enable medical coders to report specific variations in a procedure or medical service outside of the standard definition . This added detail is essential for accurate billing, reimbursement, and avoiding audits.
Why Modifier Codes are Used
Modifier codes serve several important purposes:
- Specify service variations : Modifiers indicate if the procedure was altered from the stated CPT definition . This could involve different site, technique, multiple procedures, or other variations.
- Indicate additional services : Modifiers can convey when additional services are provided during the same session as a primary procedure. For instance, repairing incidental damage during surgery.
- Prevent denied claims : Modifiers supply the details needed to demonstrate medical necessity and support reimbursement for certain services.
- Bypass edits : Some modifiers override National Correct Coding Initiative (NCCI) edits to allow payment of service combinations normally bundled or not allowed.
- Meet payer requirements : Many payers require particular modifiers to be appended to certain codes before they will reimburse it.
In summary, modifiers add clarity and details needed for accurate billing, reimbursement, and avoiding lengthy appeals or audits down the road. Applying modifiers judiciously is a key component of compliant coding.
Common Types of Modifier Codes
With over 340 different modifiers in use today, it can be overwhelming to understand when and how to apply them accurately.
We’ll break down some of the most common modifier categories with examples:
Anatomic modifiers indicate the body site or part where a procedure was performed.
Using these modifiers is essential since many CPT codes can be performed on different areas, which impacts billing:
- Eyes and Eyelids : -LT (left) , -RT (right) , -E1 (upper left) , -E2 (lower left) , -E3 (upper right) , -E4 (lower right)
Example: 67810 – Repair of ectropion; excision tarsal wedge -E1 (upper left eyelid)
- Digits : -FA (fingers) , -TA (toes) , -F1-F9 (specify finger) , -T1-T9 (specify toe)
Example: 26850 – Hammertoe operation; one toe -T2 (second toe)
- Limbs : -LC (left circumferential) , -RC (right circumferential) , -LD (left distal) , -RD (right distal) , -LP (left proximal) , -RP (right proximal)
Example: 27524 – Repair, tendon or muscle; rotator cuff -RC (right shoulder)
Careful use of anatomic modifiers eliminates any ambiguity about which body part was treated.
Global Surgery Modifiers
Global surgery modifiers are crucial to convey the specific services provided during complex surgical cases:
- -54: Surgical care only . Apply when one physician does the surgical procedure while another provides pre/post-operative management.
- -55: Post-operative management only . Used when a physician provides post-op care but was not involved in the surgery itself.
- -56: Pre-operative management only . Indicates a physician handled pre-op care but did not perform the actual surgery.
- -58: Staged/related procedure . Links two or more procedures split into different sessions of the global period.
- -78: Unrelated procedure during global period . Shows full reimbursement warranted when an unrelated procedure falls in the global window.
- -79: Unrelated procedure in post-op period . Same as -78 but used when the unrelated procedure is performed during the post-op phase only.
These modifiers are imperative to bypass global surgery package rules and obtain proper payment in complex cases with multiple providers.
Bilateral Surgery Modifiers
Bilateral modifiers should be applied when the same procedure is performed on contralateral, bilaterally symmetrical body parts:
- -50: Bilateral procedure . Reports a procedure performed bilaterally at a single session. Reimbursement varies by payer.
- -LT: Left side . Use with bilateral codes when performed on one side only.
- -RT: Right side . Same principle as -LT but for the right side only.
Some payers prefer billing bilateral procedures on two separate line items with -LT and -RT modifiers rather than using -50 . Check payer policies to ensure accurate billing.
Repeat/Multiple Procedure Modifiers
These modifiers indicate repeat or multiple procedures:
- -76: Repeat procedure . Identifies a procedure repeated by the same physician on the same date.
- -77: Repeat procedure by another physician . Codes a procedure repeated by a different physician on the same day.
- -59: Distinct procedural service . Documents a distinct procedure separate from the primary procedure or service.
Proper application of these modifiers helps bypass edits for repeat services and ensures maximum reimbursement.
Assistant Surgeon and Co-Surgeon Modifiers
Modifiers for surgical assistants and co-surgeons include:
- -80: Assistant surgeon . Denotes a procedure where an assistant surgeon participated. Reimbursement percentage varies by payer.
- -81: Minimum assistant surgeon . Used when an assistant surgeon assisted on only a small portion of the procedure. Reduced payment applies.
- -62: Co-surgeon . Indicates two surgeons worked together as primary surgeons performing distinct parts of a procedure. Each surgeon bills the full procedure code with this modifier.
Understanding when to apply these modifiers prevents payment issues for surgical assistance services.
Significant Procedure Modifiers
These modifiers identify significant or highly complex procedures that may warrant added reimbursement:
- -22: Increased procedural service . Documents substantial additional work required beyond what is conveyed by the base code.
- -52: Reduced services . Indicates a procedure was reduced or eliminated due to extenuating circumstances discovered during the procedure.
Use these modifiers judiciously when the procedure performed was significantly different than normal for that code based on objective evidence in the medical record.
When to Use Modifiers
With hundreds of modifiers to choose from, the key is understanding accurate usage principles:
- Never use modifiers just to bypass edits . Modifiers should only be applied when the procedure legitimately meets modifier criteria.
- Do not overuse modifiers . Use them only when the medical record clearly documents the specific variation in procedure or service.
- Check payer guidelines . Many payers publish lists of procedures requiring certain modifiers and rules for reimbursement.
- Use specific anatomic modifiers whenever a procedure is performed on a non-typical site as defined by the code.
- Apply repeat/multiple procedure modifiers any time the same procedure is repeated or multiple procedures performed at the same session.
- Use bilateral modifiers when the identical procedure is performed bilaterally at the same session.
- Clarify surgeries involving surgical teams, concurrent procedures, and staged operations with appropriate global surgery modifiers.
- Indicate assistant or co-surgeon participation using the correct corresponding modifiers.
- Highlight unusual circumstances using modifiers like increased/decreased procedural service when very distinct from the norm.
In general, modifiers should be applied when needed to accurately communicate details that affect coding, billing, and reimbursement. Using them improperly can lead to fraudulent billing allegations. When in doubt, err on the side of not using modifiers versus misusing them.
Examples of Proper Modifier Usage
Below we’ll explore examples of appropriate modifier application in specific medical coding scenarios:
Scenario : A patient undergoes excision of a thigh lipoma on the left proximal thigh.
CPT code billed :
- 23915 – Neoplasm, soft tissue of lower extremity; excision
Modifier used : -LP (left proximal)
Reason : The excision of a left proximal thigh lipoma matches the -LP anatomic site modifier . Anatomic modifiers should be used any time the procedure is performed on a different body part than what is typical for that code.
Repeat Procedure Modifiers
Scenario : A patient returns to the ER with chest pain 2 days after initial treatment. A repeat EKG is performed during the second ER visit.
CPT codes billed :
- 93000 – Electrocardiogram, routine ECG with at least 12 leads; interpretation and report only
- 93000-76 – Electrocardiogram, routine ECG with at least 12 leads; interpretation and report only (repeat procedure by same physician)
Modifier used : -76 (repeat procedure by same physician)
Reason : The repeat EKG on the follow-up ER visit for chest pain is appropriately identified by appending modifier -76 to the second 93000 code.
Scenario : A patient undergoes bilateral knee arthroscopies with meniscectomy during the same surgery.
- 29881 – Arthroscopy, knee, surgical; with meniscectomy (medial OR lateral)
- 29881-50 – Arthroscopy, knee, surgical; with meniscectomy (medial AND lateral)
Modifier used : -50 (bilateral procedure)
Reason : Billing the meniscectomy CPT code on two separate lines with modifier -50 indicates this procedure was performed bilaterally during one surgical session.
Scenario : Dr. Smith performed a hip replacement surgery. Dr. Jones provided the post-operative hospital follow up care.
- 27130 – Total hip arthroplasty
- 99024 – Postoperative follow-up visit, normally included in surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason(s) related to the original procedure.
Modifier used : -55 (post-operative management only)
Reason : Modifier -55 conveys Dr. Jones handled post-op care after Dr. Smith completed the actual hip replacement surgery. This modifier bypasses global surgical package rules to allow both physicians to be reimbursed for their distinct services.
These examples demonstrate the importance of properly assigning modifiers to avoid denied claims and receive appropriate payment. Take time to learn modifier definitions and payer billing requirements related to their use.

Inappropriate Use of Modifiers
While modifiers are invaluable for reporting special circumstances, there are also inappropriate ways they are sometimes misused:
- Appending modifiers to bypass edits when there is no supporting medical documentation.
- Using modifiers improperly to obtain higher reimbursement.
- Failing to use modifiers when required to convey special circumstances impeding reimbursement.
- Overusing modifiers on every claim whether they are warranted or not.
- Assigning modifiers randomly without verifying correct usage.
- Applying modifiers contradictory to CPT definitions or payer policies.
- Listing modifiers that do not provide added value or useful information.
- Using modifiers without linking them to the appropriate procedure code.
- Unbundling codes and adding modifiers to gain higher payment when a comprehensive code should be billed instead.
To summarize, modifiers must be applied accurately and ethically based on documentation in the medical record. Incorrect use of modifiers to influence reimbursement is considered fraud .
Auditing Modifier Usage
Given the complexity of modifier rules and potential for misuse, regular auditing is essential:
- Verify documentation – Audit a sample of records where modifiers were applied to ensure appropriate use is clearly documented in the medical record.
- Check billing accuracy – Review operative reports and other documentation to confirm billed procedures, diagnoses, and modifier usage match what was actually performed/documented.
- Compare modifier percentages – Compare use of modifiers as a percentage of total claims against historical baselines and watch for unusual increases.
- Assess high-usage areas – Conduct regular risk analysis of procedures, providers, and modifier types with frequent or disproportionate use.
- Review denials – Analyze reasons for denied claims related to modifier use and improper documentation.
- Provide education – Offer additional training on modifiers to departments/providers with higher incidence of incorrect usage.
Proactive auditing helps fix issues early before they become ingrained habits leading to compliance headaches. It also provides valuable physician education on proper modifier use.
Modifier Codes Must be Used Ethically and Correctly
In summary, modifier codes play a vital role in reporting important details to facilitate reimbursement and avoid delays. However, they must be applied precisely according to usage rules and medical record documentation. Incorrect use of modifiers to influence higher payment is illegal .
Healthcare providers should cultivate a culture of coding integrity where modifiers are used properly to convey true variations in services . Take time to fully understand when modifiers are warranted based on payer billing rules and documentation. Perform regular auditing to validate appropriate modifier usage. With an ethical approach, modifiers enable accurate billing and optimal reimbursement for medically necessary services .
Modifier codes provide the details needed for accurate billing and reimbursement. However, to leverage them effectively requires an in-depth understanding of appropriate usage based on medical necessity , CPT definitions , payer policies , and documentation .
Use this comprehensive guide as a resource when questions arise about when and how to apply modifiers.
Key takeaways include:
- Modifiers enable reporting of important variations in procedures and services.
- Hundreds of modifiers exist, with common types including anatomic, global surgery, bilateral, repeat, assistant surgeon, and significant procedure modifiers.
- Modifiers should only be used when supported by documentation and medical necessity.
- Inappropriate use of modifiers to bypass edits or increase payment is fraudulent.
- Regular auditing helps ensure modifiers are applied properly according to usage rules.
- Ongoing training is key to consistent ethical application of modifiers.
With the intricate modifier guidelines, it’s normal for questions to surface. Reach out to experienced coding professionals when unsure if a modifier is warranted.
Correct modifier usage ultimately facilitates proper reimbursement for clinically appropriate services rendered . This improves revenue cycle management and helps avoid lengthy claim appeals, audits, or even allegations of fraudulent billing . By using modifiers ethically based on established rules and documentation, providers can optimize payment while demonstrating coding integrity.

CPT Medical Modifiers
Understanding the significance of cpt modifiers in medical coding.
In the realm of medical coding, precision is paramount. Accuracy ensures that healthcare providers are reimbursed correctly for the services they render and that patients receive appropriate care without encountering billing discrepancies. Within the Current Procedural Terminology (CPT) coding system, modifiers play a crucial role in refining the coding process, providing additional information about the services or procedures performed. Let’s delve into why CPT modifiers are indispensable in medical coding .
Enhancing Specificity
Differentiating services, addressing unforeseen circumstances, compliance and documentation.
One of the primary functions of CPT modifiers is to provide additional specificity to a procedure or service. In many cases, medical procedures may have unique circumstances or complications that aren’t fully captured by the standard CPT codes. Modifiers allow healthcare professionals to convey these nuances, ensuring that the coding accurately reflects the complexity of the service provided.
For example, let’s consider a simple surgical procedure such as a knee arthroscopy. While the standard CPT code may cover the basic procedure, the addition of a modifier can indicate if the surgery was performed on the left or right knee, or if it involved a bilateral procedure. This level of detail is essential for accurate billing and tracking of patient care.
In some instances, medical procedures may appear similar but have distinct differences that impact coding and billing. CPT modifiers help differentiate between these services, preventing confusion and ensuring proper reimbursement.
For instance, imagine a scenario where a patient undergoes a surgical procedure to repair a fracture. Depending on the complexity of the fracture and the method of repair, different CPT codes may apply. By appending the appropriate modifier, such as indicating whether the fracture repair was performed with an open or closed technique, medical coders can accurately capture the nature of the service rendered.
Medical procedures don’t always go according to plan. Complications may arise during surgery, or additional services may be required unexpectedly. CPT modifiers allow healthcare providers to communicate these unforeseen circumstances in their coding, ensuring that they receive appropriate compensation for the extra time, resources, and expertise invested in patient care.
For example, during a routine cataract surgery, the surgeon may encounter unexpected complexities that require additional surgical techniques or equipment. By appending a modifier to the standard CPT code, the coder can convey the unique circumstances of the procedure, facilitating accurate billing for the additional services rendered.
In addition to facilitating accurate reimbursement, CPT modifiers also play a crucial role in compliance and documentation. Healthcare organizations must adhere to coding guidelines established by regulatory bodies such as the Centers for Medicare & Medicaid Services (CMS). Proper use of modifiers ensures that coding practices align with these guidelines, reducing the risk of audits, denials, and potential penalties.
Furthermore, modifiers serve as valuable documentation tools, providing a clear record of the specific circumstances surrounding each medical procedure. This documentation not only supports accurate billing but also contributes to comprehensive medical records, aiding in patient care continuity and clinical decision-making.
In the intricate landscape of medical coding, CPT modifiers serve as indispensable tools for precision, differentiation, and compliance. By enhancing specificity, addressing unforeseen circumstances, and facilitating accurate documentation, these modifiers play a vital role in ensuring that healthcare providers are reimbursed correctly for the services they deliver and that patients receive the care they need. Understanding the importance of CPT modifiers is essential for medical coders, healthcare professionals, and healthcare organizations striving for excellence in coding accuracy and billing integrity.
Common CPT Modifiers
Anesthesia has its own modifiers that correspond to a patient’s health condition:
- P1 – Normal, Healthy Patient
- P2 – Patient with Mild Systemic Disease
- P3 – Patient with Severe Systemic Disease
- P4 – Patient with Severe Systemic Disease That is a Constant Threat to Life
- P5 – Moribund patient who is not expected to survive without the operation
- P6 – Declared brain-dead patient whose organs are being removed for donor purposes
Review the proper use of each modifier. Understand when each modifier should be applied.
- Procedure has both a professional and technical component
- Service is performed by more than 1 physician and/or in more than 1 location
- Service has been increased or reduced
- Only part of a service was performed
- An adjunctive service was performed
- Service or procedure was provided more than once
- Unusual events occurred
- Service was provided during a global period but is NOT included as part of the global reimbursement
CPT Modifier 22- Increased Procedural Services
Documentation must support the substantial additional work and the reason for the additional work, which may include:
- Increased intensity Time
- Technical difficulty of procedure
- Severity of patient’s condition
- Physical and mental effort required
- Your documentation should provide our reviewers with a clinical picture of the patient; the procedures/services performed and support the use of modifier 22. Depending on the documentation, we may or may not allow additional reimbursement.
- Do not append modifier 22 to an E/M (Evaluation & Management) service; only report it with procedure codes that have a global period of 0, 10, or 90 days.
CPT Modifier 23- Unusual Anesthesia
- Modifiers may only be submitted with anesthesia procedure codes (i.e., CPT codes 00100-01999).
- Diagnostic bronchoscopy for mentally ill patients who become combative
CPT Modifier 24- Unrelated Evaluation and Management Service by the Same Physician or Other Qualified
Modifier 24 is defined as an unrelated evaluation and management service by the same physician or other qualified health care professional during a post-operative period. Medicare defines same physician as physicians in the same group practice who are of the same specialty. In this instance they must bill and be paid as though they were a single physician.
Modifier 24 is applied to two code sets:
- Evaluation and management (E/M) services (99202-99499).
- General ophthalmological services (92002-92014), which are eye examination codes.
- For unrelated critical care during the post-operative period refer to the FT modifier.
- Appropriate use
- Use Modifier 24 with the appropriate level of E/M service.
Use Modifier 24 on an E/M when:
An unrelated E/M service is performed beginning the day after the procedure, by the same physician, during the 10 or 90-day post-operative period. Documentation indicates the service was exclusively for treatment of the underlying condition and not for post-operative care. The same physician is managing immunosuppressant therapy during the post-operative period of a transplant. The same physician is managing chemotherapy during the post-operative period of a procedure. The same diagnosis as the original procedure could be used for the new E/M if the problem occurs at a different anatomical site. Inappropriate use
Do not use Modifier 24 when:
- The E/M is for a surgical complication or infection, removal of sutures, or other wound treatment. These treatments are part of the surgery package.
- The surgeon admits a patient to a skilled nursing facility for a condition related to the surgery.
- The medical record documentation clearly indicates the E/M is related to the surgery. Outside of the post-op period of a procedure.
- Services are rendered on the same day as the procedure.
- Reporting exams performed for routine postoperative care.
- Reporting surgical procedures, labs, x-rays, or supply codes.
- Health Care Professional During a Postoperative Period
CPT Modifier 25- Significant, Separately Identifiable Evaluation and Management Service by the Same Physician or Other Qualified Health Care Professional on the Same Day of the Procedure or Other Service
- Often questions are posed regarding whether to bill an E/M visit on the same day as a procedure and/or other services with modifier 25.
- Are there signs, symptoms, and/or conditions the physician or the other qualified health care professional must address before deciding to perform a procedure or service?
- If Yes, based on the documentation, an E/M service might be medically necessary with modifier 25
- Were the physician’s or other qualified health care professional’s evaluation and management of the problem significant and beyond the normal preoperative and postoperative work?
- If Yes, an E/M may be billed with modifier 25
- If No, it is not appropriate to bill with modifier 25
CPT Modifier 26- Professional Component
- Modifier 26 is defined as the professional component (PC).
- The PC is outlined as a physician’s service, which may include technician supervision, interpretation of results and a written report.
- Use modifier 26 when a physician interprets but does not perform the test.
- Most radiology codes, including ultrasounds, x-rays, CT scans, magnetic resonance angiography, and magnetic resonance imaging, may be billed with modifier 26 or TC, or with no modifier at all, indicating that the provider performed both the professional and technical services. indicates that a physician has interpreted the results of a test when they did not personally perform it. Modifier 26 is the professional component (PC) of a procedure. The PC is outlined as a physician’s service, which may include technician supervision, interpretation of results, and a written report.
- Is appended to billed codes to indicate that only the professional component of a service/procedure has been provided. For example, if a facility provides the technical component of a service/procedure, while an individual physician performs the professional component, they should report the code with modifier -26.
- Modifier 26 should always be added before any other modifier
- This modifier must be reported in the first modifier field.
Appropriate use of Modifier 26
- When billing only the professional component portion of a test
- To report the physician’s interpretation of a test
- Procedures that have a “1” in the Professional Component (PC)TC field on
- the Medicare Physician Fee Schedule Database (MPFSDB)
Procedures falling into the following types of service:
1 – medical care/injections 2 – surgery 4 – radiology 5 – lab 6 – radiation therapy 8 – assistant surgeon, inappropriate use of modifier 26:.
- Evaluation and management (E/M) or anesthesia codes Procedure or service descriptors that indicate professional component only
- Global test only codes, example: CPT 93000.
- Professional component only codes. PC/TC indicator 2 of MPFSDB denotes a professional component only code that identifies stand-alone codes.
- An example of a professional component only code is 93010, Electrocardiogram; interpretation and report. Modifier 26 cannot be used with this code.
- Re-read results of an interpretation provided by another physician.
CPT Modifier 27-Multiple Outpatient Hospital E/M Encounters on the Same Date
- Append modifier 27 when reporting multiple outpatient hospital evaluation and management (E/M) services on the same date.
- Modifier 27 was created exclusively for hospital outpatient departments (ex. hospital emergency department, clinic, and critical care).
- Note: Physician practices may not use this modifier. This modifier should only be reported on the UB-04 Part A claim form or electronic equivalent.
- Hospitals may append modifier 27 to the second and subsequent E/M code to indicate that the E/M service is a “separate and distinct E/M encounter” from the service previously provided that same day in the same or different hospital setting.
- 92002-92014 (Ophthalmological E/M services)
- 99281-99285 (Hospital type A emergency department visits)
- 99291-99292 (Critical care)
- G0175 (Interdisciplinary team conference)
- G0380-G0384 (Hospital type B emergency department visits)
- G0402 (Initial preventive physical examination)
- G0463 (Hospital outpatient clinic visit for assessment and management)
- Report condition code G0 (zero) with modifier 27 when multiple medical visits occur on the same day in the same revenue centers.
CPT Modifier 32 – Mandated Services
Is used only whenever a service has to be extended to a third party entity or in the case of Worker’s Compensation or some other such official entity. However, modifier 32 may never be used when the patient wishes to seek a second opinion from a different doctor.
CPT Modifier 33 – Preventative Services
Used to identify medical care whose primary purpose is delivery of an evidence-based service, based on recommendations from the US Preventive Services Task Force.
CPT Modifier 47 – Anesthesia by Surgeon
This modifier may be submitted when the operating surgeon performs the anesthesia service (does not include local anesthesia). Add CPT modifier 47 to the basic service for regional or general anesthesia provided by the surgeon.
CPT Modifier 50 – Bilateral Procedures
- Modifier 50 is used to report bilateral procedures that are performed during the same operative session by the same physician.
- These procedures can be performed on both sides of the body, such as the spine, skull, or nose.
- Modifier 50 is used as a payment modifier, rather than an informational modifier. It can affect payment depending on the procedure code and the BILAT SURG indicator.
- Modifier 50 can be used when two procedures are reported using the same CPT code and are performed on both sides of a single, symmetrical structure or organ. For example, modifier 50 can be used when two procedures on the spine or skull are performed using the same CPT code.
- Modifier 50 is not reported when a procedure is identified as bilateral or unilateral
CPT Modifier 51 – Multiple Procedures (some multiple surgical procedures must be reported WITHOUT modifier 51 identified as add-on codes – appendix I)
• Modifier 51 is used to indicate that the same provider performed multiple procedures on the same day during the same session. This includes procedures other than E/M services, such as physical medicine and rehabilitation services or supplies. • Modifier 51 is a Medicare contractor assigned modifier. Medicare does not recommend reporting modifier 51 on your claim submission. • You should list the most resource-intense (highest paying) procedure first, and append modifier 51 to the second and subsequent procedures • Multiple surgeries performed on the same day, during the same surgical session. • Diagnostic Imaging Services subject to the Multiple Procedure Payment Reduction that are provided on the same day, during the same session by the same provider. • Note: Medicare doesn’t recommend reporting Modifier 51 on your claim; our processing system will append the modifier to the correct procedure code as appropriate.
Appropriate Usage of CPT Code Modifier 51
- The same physician performs more than one surgical service at the same session (Indicator 2)
- The technical component of multiple diagnostic procedures, Multiple Procedure Payment Reduction (MPPR) rule applies (Indicator 4).
- The multiple surgical procedures are done on same day but billed on two separate claims.
- The surgical procedure code is the lower physician fee schedule amount.
- The diagnostic imaging procedure with the lower technical component fee schedule amount.
Inappropriate Use of CPT Code Modifier 51
- Do not append to add-on codes (See Appendix D of the CPT manual)
- Do not report on all lines of service
- Do not append when two or more physicians each perform distinctly, different, unrelated surgeries on the same day to the same patient. Additional Information
- Medicare pays for multiple surgeries by ranking from the highest physician fee schedule amount to the lowest physician fee schedule amount.
- 100% of the highest physician fee schedule amount
- 50% of the physician fee schedule amount for each of the other codes
- Medicare will forward the claim information showing Modifier 51 to the secondary insurance.
- Multiple surgery pricing also applies to assistant at surgery services.
- Multiple surgery pricing applies to bilateral services (modifier 50) performed on the same day with other procedures.
CPT Modifier 52 – Reduced Services
Under certain circumstances a service or procedure is partially reduced or eliminated at the provider’s discretion.
- Modifier 52 is used to indicate a partial reduction or discontinuation of radiology procedures or services that do not require anesthesia. This can be used when a physician elects to partially reduce or discontinue a procedure for reasons other than the patient’s well being being threatened.
- Modifier 52 is outlined for use with surgical or diagnostic CPT codes. It can be used when a procedure has an existing CPT code, but not all of the components of the code were performed. For example, if the patient only receives 30 minutes of PT instead of the 45 minutes that was scheduled.
- Procedure codes submitted with modifier 52 will be reimbursed at a reduced rate. Health plans reimburses procedure(s) appended with modifier 52 at 50% of the allowable amount
Appropriate usage of CPT Code 52 – Reduced Services
- The service performed was significantly less than usually required.
- To indicate partial reduction of services for which anesthesia is not planned.
- Append modifier to the reduced procedure’s CPT code.
- Ambulatory surgical centers (ASC) use modifier 52 to indicate the discontinuance of a procedure not requiring anesthesia.
- Contractors apply a 50 percent payment reduction for discontinued radiology and other procedures not requiring anesthesia.
- ASC services billed with modifier -52 modifier are not subject to the multiple procedure reduction.
Inappropriate Use of CPT Code 52 Reduced Services
- To report the termination of a procedure.
- Do not use on time-based codes.
- When used on evaluation and management services. Supporting documentation
- Additional information to support the modifier can be written in the narrative of claim
- If data cannot be written in the narrative, documentation must be submitted.
- Supporting documentation should:
- State when the procedure was started.
- Explain why the procedure was discontinued.
- Notate the percentage of the procedure that was performed.
CPT Modifier 53- Discontinued Procedure
Under certain circumstances, the provider may elect to terminate a surgical or diagnostic procedure due to circumstances that may threaten the wellbeing of the patient.
Appropriate Use of CPT Modifier 53
- A discontinued procedure after induction of anesthesia.
- Append modifier to the discontinued procedure’s CPT code. Inappropriate usage
- Reporting on an evaluation and management (E/M) procedure code
- Discontinued surgeries prior to the administration of anesthesia
- Do not use on time-based procedure codes (i.e., anesthesia, critical care and psychotherapy)
- Used for services in an ambulatory surgery center or a hospital outpatient department Supporting documentation
CPT Modifier 54 – Surgical Care Only & 55- Postoperative Management Only
Global package.
- Physicians who perform the surgery and furnish all the usual pre- and postoperative work should bill for global surgical care by using the proper CPT surgical code(s). In this situation physicians should not bill separately for visits or other services that are included in the global package. No modifier is necessary.
- When different physicians in a group practice participate in the care of the patient and all the physicians reassign benefits to the group, the group bills for the entire global package. The physician who performs the surgery is shown as the performing physician. No modifier is necessary
Co-management
- Occasionally a physician must transfer the care of the patient during the global care period. In these instances, the use of a modifier will be necessary to distinguish who is providing care for the patient. Novitas expects these instances to be rare.
Reasons for splitting care
- The operating surgeon is unavailable after surgery and the patient’s postoperative care has to be managed by another physician.
- The patient is unable to travel the distance to the surgeon’s office for postoperative care visits.
- The care is provided in a health professional shortage area (HPSA) and the patient is unable to travel to the surgeon’s office.
- The surgeon practices in a site remote from where the patient recuperates, e.g., the surgery is performed in a remote area and the surgeon does not return to the area frequently enough to provide the preoperative or postoperative care.
- The patient voluntarily wishes to be followed postoperatively by another physician.
- The surgery is performed by an itinerant surgeon in a remote area of the country.
Transfer of postoperative care is not covered if
- The operating surgeon is available, and he/she can manage other patients postoperatively unless the patient voluntarily wishes to be followed postoperatively by another provider.
- The surgeon does follow the patient postoperatively but splits the fee with another provider.
- Two or more physicians co-manage patients indiscriminately as a matter o policy and not on a case-by-case basis.
- A physician demands to manage the postoperative care and indicates that he/she will withhold making referrals to surgeons who would not agree to split global surgery payments.
- A surgeon opts to transfer postoperative care.
- The transfer is not made in writing.
- The transfer of care is used as an incentive for obtaining referrals from providers to receive postoperative care reimbursement.
- The patient has not consented to the transfer of care even after being apprised of the medical and/or logistic advisability or the risks and benefits of transfer care.
Surgical care for CPT Modifier 54
- Specific billing guidelines must be followed when the surgical procedure and post-operative care is split between different physicians. Modifiers 54 and 55 are used to indicate two different physicians are rendering the surgical care and post-operative management services. Where physicians agree on transfer of care during a 10-day or 90-day global period, the following modifiers are used:
- 54 for surgical care only, or
- 55 for postoperative management only
- One-day preoperative care
- Intraoperative services
- Any in-hospital visits
- Date of the surgery
- Procedure code for the surgery
- 54 modifier to indicate that the bill is reflective only of the surgical care
- If the physician who performed the surgery relinquishes care any time after the surgery, the date of the transfer of care must be indicated in item 19 or the equivalent for electronic submission.
Postoperative/Out of hospital care for CPT Modifier 54
Bill services with:.
- 55 modifier
In the case where the surgeon also cares for the patient for some period following discharge, the surgeon should bill the surgery with a 55 modifier and indicate the portion of the post-operative care provided in addition to the surgery with a 54 modifier (to indicate the intra-operative service). In those cases where the postoperative care is “split” between physicians, the billing for the postoperative care should be reported as follows:
- Report the date of service using the date of the surgical procedure.
- Report the procedure code for the surgical procedure, followed by modifier 55.
- Report the date the post-operative care began and ended along with the number of post-operative care days in the narrative field of electronic claims, or item 19 on the CMS 1500 claim form or the electronic equivalent.
- When there is a transfer of postoperative care, Medicare regulations require a written transfer of care agreement between the operating surgeon and the physician assuming care. Both the surgeon and the physician(s) providing the post-operative care must keep a copy of the written transfer agreement in the beneficiary’s medical records.
- Where a transfer of postoperative care occurs, the receiving physician cannot bill for any part of the global services until he/she has provided at least one service. Once the physician has seen the patient, that physician may bill for the period beginning with the date on which he/she assumes care of the patient using the surgery date as the billed date of service.
Both bills for surgical care only and postoperative care only, must contain:
- Same date of service
- Same surgical procedure code
- Appropriate modifier
- Note: Providers must report the date when post-operative care is assumed from another provider including the date post-operative care began and ended along with the number of post-operative care days provided in the narrative field on electronic claims, or item 19 on the CMS 1500 claim form. This will facilitate processing of the claim and reduce unnecessary rejections.
CPT Modifier 56 – Preoperative Management Only
Is used by a physician or other qualified healthcare professional who performs preoperative care but does not provide the intraoperative (Surgical) or postoperative services.
CPT Modifier 57 – Decision for Surgery
Cpt modifier 57 is used to:.
Indicate that documentation is available in the patient’s records to support the E/M service. Modifier 57 is used to indicate an Evaluation and Management (E/M) service resulted in the initial decision to perform surgery either the day before a major surgery (90 day global) or the day of a major surgery.
Appropriate Use of CPT Modifier 57
Append, only to the E/M procedure code, where the decision to perform surgery is made the day of or day before a major surgery during an E/M service.
Inappropriate Use of CPT Modifier 57
- Appending to a surgical procedure code.
- Appending to an E/M procedure code performed the same day as a minor surgery.
- When the decision to perform a minor procedure is done immediately before the service, it is considered a routine preoperative service and not billable in addition to the procedure.
- Do not report on the day of surgery for a preplanned or prescheduled surgery.
- Do not report on the day of surgery if the surgical procedure indicates performance in multiple sessions or stages.
Global period includes:
- Day before surgery
- Day of the surgery; and
- Note: A major surgery has a 90 day post-operative period and a minor surgery has either a zero or a 10 day post-operative period.
- Preoperative period is the day before the surgery or the day of surgery E/M service resulting in initial decision to perform major surgery is furnished during post-operative period of another unrelated procedure, then the E/M service must be billed with both the 24 and 57 modifiers.
CPT Modifier 58- Staged or Related Procedure or Service by the Same Physician During the Postoperative Period
Planned, either at the time of the first procedure or prospectively • More extensive than the first procedure • A new postoperative period begins when the staged procedure is billed. Appropriate use Report when a procedure or service during the postoperative period was: • Planned prospectively or at the time of the original procedure. • More extensive than original procedure. • For therapy following a diagnostic surgical procedure. • When performing a second or related procedure during the postoperative period. Inappropriate use • Staged procedures do not apply to claims for assistant at surgery. • Appending the modifier to ambulatory surgical center (ASC) facility fee claims. • Doesn’t apply to procedures with XXX global period. • Unrelated procedures during the postoperative period. • Reporting the treatment of a complication from original surgery that requires a return to operating room or service not separately payable that does not require a return to the operating room.
59- Distinct Procedural Service
This means that a procedure or service was distinct or independent from other services performed on the same day. Modifier 59 is used for procedures or services that are not normally reported together, but are appropriate and separately billable given the circumstances.
Modifier 59 can be used to distinguish:
- A different session or patient encounter
- A different procedure or surgery
- A different anatomical site
- A separate injury
- When an intravenous (IV) protocol calls for two separate IV sites
CPT Modifier 62 -Two Surgeons
- Indicates when two surgeons work together as primary surgeons on a single reportable procedure. Each surgeon must add modifier 62 to the same procedure code. Modifier 62 indicates that two or more surgeons were required for the same procedure on the same patient, during the same operative session, and on the same date of service.
- For example, modifier 62 would be used when one surgeon makes an incision and exposes the area requiring surgery, and another surgeon performs the surgery. Modifier 62 can also be used for co-surgery, where two surgeons perform parts of a procedure simultaneously, such as a heart transplant.
- Modifier 62 must be on both claims. If it is not, one physician will be paid at 100% and the other physician’s claim will be denied.
- Medical records must demonstrate why a co-surgeon or assistant was needed during the surgery.
CPT Modifier 63- Procedure Performed on Infants less than 4 kg.
Represents procedures performed on neonates and infants up to a present body weight of 4 kilograms.
CPT Modifier 66- Surgical Team
- If a team of surgeons (more than two surgeons of different specialties) is required to perform a specific procedure, each surgeon bills for the procedure with a modifier 66.
- Documentation is required to support claims submitted with this modifier.
- Note: The documentation should include each surgeon’s description of their role in the performance of the surgery.
Correct Use of CPT Modifier 66
- Includes other highly skilled and specially trained personnel
- Includes different types of complex equipment
- Usually confined to organ transplant teams
- Reimbursed “by report”
- 0 – Team surgeons not permitted for this procedure.
- 1 – Team surgeons could be paid; supporting documentation required to establish medical necessity of a team; pay by report.
- 2 – Team surgeons permitted; pay by report.
Every surgeon must append modifier 66 to the CPT code.
Incorrect Use CPT Modifier 66
CPT Modifier 66 should not be used for two or less surgeon
CPT Modifier 73- Discontinued Outpatient Hospital/Ambulatory Surgery Center (ASC)
Procedure Prior to the Administration of Anesthesia
Physicians should not use this modifier.
This is only appropriate for use by the ASC.
Appropriate Usage of CPT Modifier 73
Due to extenuating circumstances or threaten patient well-being:
- Prior to procedure started/patient’s surgical preparation (including sedation or taken to procedure room)
- Prior to administration of anesthesia (local, regional block or general)
Inappropriate Usage of CPT Modifier 73
- Physician cancelled the surgical or diagnostic procedure prior to administration of anesthesia and/or surgical preparation of the patient
- Elective cancellation of a procedure
- Surgeon cancels or postpones because patient complained of a cold or flu upon intake
CPT Modifier 74- Discontinued Outpatient Hospital/Ambulatory Surgery Center (ASC) Procedure After the Administration of Anesthesia
- The patient must be prepared for the procedure and taken to the room where the procedure is to be performed
- This modifier is not for physician use. It is only appropriate for the ASC.
- For physician reporting of discontinued procedures, refer to modifier 53.
Appropriate usage of CPT Modifier 74
- may terminate surgical/diagnostic procedure after procedure starts (incision made, intubation started, scope inserted), and after administration of anesthesia (local, regional block or general).
Inappropriate usage of CPT Modifier 74
- Elective cancellation or postponement of a procedure based on the physician or patient’s choice
- Termination of the procedure prior to the beginning of the procedure or the administration of anesthesia
CPT Modifier 76 -Repeat Procedure by Same Physician or Other Qualified Health Care Professional
- Modifier 76 defines a repeat procedure or service, on the same day, by the same physician or other qualified healthcare professional (QHP).
- Use modifier 76 to indicate a procedure or service was repeated subsequent to the original procedure or service.
- Use modifier 76 on a separate claim line with the number of repeated services.
- Do not report modifier 76 on multiple claim lines, to avoid duplicate claim line denials.
- Bill all services performed on one day on the same claim, to avoid duplicate claim denials.
- Documentation must support the use of the modifier.
CPT Modifier 77- Repeat Procedure by Another Physician or Other Qualified Health Care Professional
Modifier 77 is defined as a repeat procedure or service by another physician or other qualified healthcare professional. Used to indicate a procedure or service was repeated by another physical or other qualified healthcare professional. Indicate that a basic procedure or service had to be repeated.
Appropriate uses of CPT Modifier 77
- Add modifier 77 to the professional component of an x-ray or electrocardiogram (EKG) procedure when the patient has two or more tests and/or more than one physician provides the interpretation and report.
- We will reimburse a second interpretation of the same EKG or x-ray only under unusual circumstances, such as:
- A questionable finding for which the physician performing the initial interpretation believes another physician’s expertise is needed, or
- A change in diagnosis resulting from a second interpretation
- Note: Absent these circumstances, we will reimburse only the interpretation and report that directly contributed to the diagnosis and treatment of the individual patient.
Inappropriate uses of CPT Modifier 77
- Billing for multiple services which are considered bundled.
- Appending Modifier 77 to an evaluation and management code.
Claim submission instructions
If performing repeat procedures on the same day:
- Report each procedure on separate lines.
- List the procedure code once by itself and then again with modifier 77.
- Do not use the units’ field to indicate the procedure was performed more than once on the same day.
- Add modifier 77 when billing for multiple services on a single day and the service cannot be quantity billed.
- Report the unusual circumstance to support the use of the modifier in the narrative description
- Failure to report modifier 77 and the unusual circumstances in the narrative portion of the claim or the EDI equivalent will result in a claim rejection.
CPT Modifier 78- Unplanned Return to the Operating Room by Same Physician or Other Qualified Health Care Professional Following Initial Procedure for a Related Procedure During the Postoperative Period
Appropriate usage of cpt modifier 78.
- To identify a related procedure (that has 10 or 90 global surgery period) requiring a return trip to the operating room within the postoperative period of a major or minor surgery.
- To treat the patient for complications resulting from the original surgery
- When the procedure code used to describe a service for a treatment of complications is the same as the procedure code used in the original procedure.
Inappropriate usage
On any procedure code that does not have global period of 0010 or 0090. • When surgery is unrelated to the original procedure. • On procedures performed in any place other than the operating room. • On ambulatory surgical center (ASC) facility services.
Facts About CPT Modifier 78
- An operating room (OR) is defined as a place of service specifically equipped and staffed for the sole purpose of performing procedures. The term includes a cardiac catheterization suite, a laser suite, and an endoscopy suite. It does not include a patient’s room, a minor treatment room, a recovery room, or an intensive care unit (unless the patient’s condition was so critical there would be insufficient time for transportation to the OR).
- Modifier 78 allows for the intraoperative percentage only of major or minor procedures (010 or 090 global periods).
- A new postoperative period does not begin when using modifier 78.
- Medicare allows codes with global surgery indicators of XXX and ZZZ in the Medicare Physician Fee Schedule (MPFS) database separately without modifier 78.
CPT Modifier 79- Unrelated Procedure or Service by the Same Physician or Other Qualified Health Care Professional During the Postoperative Period
- Modifier 79 is a pricing modifier and should be reported in the first position.
- A new post-operative period begins when the unrelated procedure is billed.
Appropriate uses of CPT Modifier 79
• To describe an unrelated surgical procedure performed during the postoperative period of the original procedure by the same physician. • When reporting identical procedures that are performed on the same day, by the same physician, but are not the same service on the same anatomical site.
Inappropriate uses of CPT Modfier 79
- The procedure performed is related to the original surgery or staged (anticipated) surgery.
- Placed on procedure codes with XXX indicator (global concept does not apply), in the global day field of the Medicare Physician’s Fee Schedule (MPFS) database.
- Reported on ambulatory surgical center (ASC) services.
- Note: If related to the original procedure, it is considered part of the global period.
CPT Modifier 80- Assistant Surgeon
- A physician, nurse practitioner, physician assistant or clinical nurse specialist who is authorized to provide such services under state law can serve as an assistant at surgery.
- The “assistant at surgery” provides more than just ancillary services. The operative note should clearly document the assistant surgeon’s role during the operative session.
- Use the “80” modifier when the assistant at surgery service was provided by a physician.
- Use the “81” This modifier pertains to physician’s services only. Minimal surgical assistance may be identified by adding the modifier 81 to the usual procedure code and describes an assistant surgeon providing minimal assistance to the primary surgeon.
- Use the “82” modifier when a qualified resident surgeon is not available in a teaching facility:
- The unavailability of a qualified resident surgeon is a prerequisite for use of this modifier and the service must have been performed in a teaching facility.
- The circumstance explaining that a resident surgeon was not available must be documented in the medical record. This modifier is not intended for use by non-physician providers.
- Use the modifier “AS” for assistant at surgery services provided by a physician’s assistant (PA), nurse practitioner (NP), or clinical nurse specialist (CNS). The provider must accept the assignment.
CPT Modifier 81- Minimum Assistant Surgeon
Modifier 81 is appended to the procedure code for an assistant surgeon who assists an operating or principal surgeon during part of a procedure. Check the Medicare Physician Fee Schedule (MPFS) Indicator/Descriptor Lists. Column A indicates if assistant at surgery is allowed.
Correct Use of CPT Modifier 81
- Append to appropriate code when more than one assistant is involved or if one person assists during a portion of surgery. Includes physicians providing minimal assistance to primary surgeon. Must be used with Type of Service 8 codes.
- This modifier identifies surgical assistant services
- Indicates exceptional medical circumstances exist
- Indicates primary surgeon has policy of never involving residents in preoperative, operative or postoperative care of his/her patients
CPT Modifier 82 – Assistant Surgeon (when qualified surgeon no available)
This modifier is used in the private insurance industry and is not commonly used in Medicare billing. Modifier 82 is only intended for use by physicians.
- This modifier is used when minimal surgical assistance is needed, but a qualified resident was not available (documentation required). First, check Medicare Physician Fee Schedule (MPFS) Indicator/Descriptor List. Column A indicates if assistant at surgery allowed/not allowed.
CPT Modifier 82 is used when:
- A qualified resident surgeon was not available to assist the primary surgeon • The service was performed in a teaching facility • Minimal surgical assistance was needed • The primary surgeon has a policy of never involving residents in the care of their patients Modifier 82 is not intended for use by non-physicians assisting at surgery, such as nurse practitioners or physician assistants. Documentation is required to support the use of modifier 82.
Correct Use of CPT Modifier 82
- Assist-at-surgery allowed with appended modifiers 80, 81 or 82
- Allowed = 16% of surgery fee schedule allowable
- Modifier 82 needs a statement that “no qualified resident surgeon was available”
- Primary surgeon must have a policy of never involving residents in preoperative, operative or postoperative care of his/her patients
- Non Physician Practitioner (NPP) or mid-level practitioner (PA, NP, CNS):
- Append AS modifier only
- Allowed equals 85% of surgical assist or 16% allowable
Incorrect Use of CPT Modifier 82
- Inappropriate to bill physician assistant surgical services with AS modifier
- Inappropriate to append modifier 58 (staging) with any assistant surgery
CPT Modifier 90- Reference (Outside) Laboratory –(Referred tests)
Is used in medical coding to indicate that a laboratory procedure was performed by a party other than the treating or reporting physician. For example, a physician might order a CBC, draw blood, and send the specimen to an outside laboratory. The laboratory bills the physician for the service.
- • Modifier 90 is appended to a procedure code. The laboratory performing the lab test must bill or submit the lab work directly. • Modifier 90 indicates pass through billing • A referring laboratory may bill for clinical laboratory tests on the clinical laboratory fee schedule performed by a reference laboratory only if the referring laboratory meets one of the following conditions: • Located in, or is part of, a rural hospital • Wholly owned by the entity performing such test. (referring laboratory wholly owns the entity performing such test, or both the referring laboratory and the entity performing such test are wholly-owned by a third entity) • Does not refer more than 30 percent of the clinical laboratory tests for which it receives requests for testing during the year (not counting referrals made under the wholly-owned condition described above)
Appropriate uses of CPT Modifier 90
- Only one laboratory may bill for a referred laboratory service.
- It is the responsibility of the referring laboratory to ensure that the reference laboratory does not bill Medicare for the referred service when the referring laboratory does.
- Referring laboratory may not bill in the event the reference laboratory bills or intends to bill Medicare.
- Must include the referring and reference laboratory’s CLIA number.
- Laboratory testing require the presence of the referring and reference laboratory’s name and address.
- The reference laboratory for a service with a 90 modifier requires the performing provider’s information.
CPT Modifier 91- Repeat Clinical Diagnostic Laboratory Test
CPT Modifier 91 Is used to indicate that a laboratory test was repeated on the same day for the same patient. This modifier is used when multiple laboratory tests are needed during a patient’s treatment, such as repeat blood glucose tests.
You should not use modifier 91 for lab tests that are repeated to confirm initial results, due to equipment or specimen malfunctions, or when another one-time code is sufficient. Modifier 91 is different from modifier 59. Modifier 59 is used when the same test is performed on different sites. For example, if two wound cultures are taken from different sites, modifier 59 would be used. Modifier 91 is used to report any repeat clinical diagnostic laboratory test being billed if:
- A single service (same CPT code) is ordered (for the same beneficiary)
- Specimen is collected more than once in a single day
- The service is medically necessary.
Appropriate Uses of CPT Modifier 91
To identify a subsequent medically necessary laboratory test on the same day of the same previous laboratory test
Inappropriate Uses of CPT Modifier 91
When there are testing problems with the specimen a more appropriate procedure code is available to describe a series of test
- Rerun of a laboratory test is done to confirm results
- Testing problems with the equipment
- Procedure code describes a series of test
- For any reason when a normal one-time result is required
Claim Submission Instructions:
- Bill all services performed same day on the same claim
- Report each service on a separate line, with quantity of one and append 91 to the repeat procedure
- Documentation must support the use of the modifier
92-Alternative Laboratory Platform Testing
CPT Modifier 92 means that the laboratory testing is performed using a kit or transportable instrument that contains a single-use disposable analytical chamber. Modifier 92 is only used with HIV testing CPT codes 86701-86703.
For example, a patient might be tested for HIV using a hand-carried transportable kit. To obtain reimbursement for performing a rapid HIV test, providers can add modifier 92 to the usual laboratory procedure CPT code for the type of HIV test.
The general order of sequencing modifiers is: Pricing, Payment, Location.
Location modifiers are coded last in all coding situations
CPT Modifier 95 – Synchronous Telemedicine Service Rendered Via a Real-Time Interactive Audio and Video Telecommunication System
CPT Modifier 95 is used to indicate a synchronous telemedicine service, or a telehealth session. This means that the service was provided through a real time audio visual conference between a patient and a provider. The provider is at a different location from the patient.
The 95 modifier is only for codes listed in Appendix P of the CPT manual. Some insurance companies, such as Medicare, accept the 95 modifier. The 95 modifier can be used with a POS of 11 to indicate that the office visit was performed via telehealth. This allows the service to be paid at 100%. Using a POS of 02 subjects the code to a facility reduction of 15%
CPT Modifier 96 – Habilitative Services
Is used when the physical therapy services are rehabilitative in nature. The CO, CQ, GO, and GP modifiers are all modifiers that indicate who performed the service
CPT Modifier 97 – Rehabilitative Services
Is used to indicate that a service or procedure was provided for rehabilitative purposes. For example, a physician or other qualified healthcare professional might add modifier 97 to a physical therapy service code to indicate that the service was rehabilitative in nature.
The Affordable Care Act (ACA) requires coverage of certain essential health benefits (EHBs), including rehabilitative and habilitative services and devices. The Current Procedural Terminology (CPT®) code 97 is a medical procedural code under the range – Provider Services and Ambulatory Service Center Modifiers.
CPT Modifier 99- Multiple Modifiers
Append modifier 99 to a procedure or service as the first modifier when there are also two or more additional modifiers applicable to the service or procedure.
Master CPT Modifiers for Flawless Medical Coding
By understanding the significance of CPT modifiers and their appropriate application, medical coders can ensure accurate representation of services rendered, optimize billing practices, and contribute to a smooth healthcare revenue cycle. This guide provides a solid foundation for mastering CPT modifiers. Remember, staying current with coding guidelines and best practices is essential for coders to excel in this ever-evolving field.
Novitas.com
https://www.aapc.com/
- Account Link Sign In
- Account Sign In
- Managing Your Practice
- Timely Topics in Payment and Practice Management
Anesthesia Payment Basics Series Codes and Modifiers
To properly and accurately report anesthesia services, one must know and adhere to rules and guidelines that are specific to anesthesia care. Additionally, the formula used to determine payment for anesthesia services is unique to anesthesia. These rules and formula may be misunderstood or improperly applied. This ASA Timely Topic is the first of a series that will break the components of anesthesia billing and payment down into individual components and provide explanation on what the components represent. Codes and Modifiers Any claim for a professional healthcare service must clearly communicate what service/procedure was performed and why is was done. To provide clarity and standardization, the Administrative Simplifications provisions within the Health Insurance Portability and Accountability Act of 1996 (HIPAA) requires all covered entities to use specially designated code sets on claims for services. Procedures and services are reported with codes and modifiers from the CPT® code set. CPT stands for Common Procedural Terminology and this code set is owned and maintained by the American Medical Association (AMA). Anesthesia codes – sometimes referred to as “ASA codes” are part of the CPT code set. Examples of CPT codes applicable to anesthesia include:
| 00790 | Anesthesia for intraperitoneal procedures in upper abdomen including laparoscopy; not otherwise specified |
| 01402 | Anesthesia for total knee arthroplasty |
As you can observe from these examples, some CPT Anesthesia codes are broad and encompass anesthesia care for a range of diagnostic or therapeutic services (eg, 00790) while others are more narrow and describe anesthesia care for limited and specific services (eg, 01402). CPT Modifier 22 – Increased Procedural Services is an example of a CPT modifier that may be used with anesthesia codes. As explained in the ASA Relative Value Guide ® (RVG™), this modifier is used to report instances of field avoidance and the increased work and complexity that follows when an anesthesiologist has limited access to the patient’s airway. The Healthcare Common Procedure Coding System (HCPCS) includes codes and modifiers that may also be used to report services or drugs and supplies when appropriate. The HCPCS code set includes several modifiers that are specific to anesthesia care and are required on claims submitted to Medicare and many other payers.
| AA | Anesthesia Services performed personally by the anesthesiologist |
| AD | Medical Supervision by a physician: more than 4 concurrent anesthesia procedures |
| QK | Medical Direction of two, three or four concurrent anesthesia procedures involving qualified individuals |
| QX | Qualified nonphysician anesthetist service: With medical direction by a physician |
| QY | Medical direction of one qualified nonphysician anesthetist by an anesthesiologist |
| QZ | CRNA service: Without medical direction by a physician |
Physician anesthesiologists report AA, AD, QK, or QY. A CRNA or Anesthesiologist Assistant reports QX; Modifier QZ is specific to CRNAs. Payers may also require HCPCS modifiers to denote monitored anesthesia care (MAC):
| QS | Monitored anesthesia care service |
| G8 | Monitored anesthesia care (MAC) for deep complex, complicated, or markedly invasive surgical procedures |
| G9 | Monitored anesthesia care for patient who has a history of server cardio-pulmonary condition |
CPT Code 00790 - Anesthesia for intraperitoneal procedures in upper abdomen including laparoscopy; not otherwise specified HCPCS Modifiers Dr A reports QK - Medical Direction of two, three or four concurrent anesthesia procedures involving qualified individuals CRNA A reports the same CPT code with modifier QX - Qualified nonphysician anesthetist service: With medical direction by a physician ICD-10-CM Code K80.01 - Calculus of gallbladder with acute cholecystitis with obstruction
On June 1, 2019, Dr. B personally provides anesthesia care for a patient undergoing a total right knee replacement.
CPT Code 01402 - Anesthesia for total knee arthroplasty HCPCS Modifier AA - Anesthesia Services performed personally by the anesthesiologist ICD-10-CM Code M17.11 - Unilateral primary osteoarthritis, right knee
Date of last update: June 12, 2024
National Medical Billing Services is excited to announce we are now nimble solutions. Learn more .
Anesthesia Coding: From CPT to Modifier, How to Code Anesthesia Services Accurately
By marcy garuccio, director of coding, anesthesia, nimble solutions .
Inaccurate coding and incomplete procedure documents are two of the top issues affecting anesthesia revenue cycle efficiency. Anesthesia coding is incredibly complex because it relies on the accuracy of procedure notes and an individual coder’s knowledge of coding guidelines.
Certified anesthesia coders know how to record the duration of procedure, the procedure’s level of difficulty, and other modifying factors that vary by payer, anesthesia provider, and anesthesia units.
nimble solution’s specialized knowledge in the anesthesia revenue cycle helps anesthesia groups regain lost revenue and maximize profitability.
In this blog, we’ll share our top 5 anesthesia coding strategies to improve revenue cycle efficiency.
1. Understand anesthesia coding guidelines
The more familiar your coding team is with anesthesia coding guidelines, such as CPT codes and time-based calculations, the more you can avoid compliance and costly claims issues.
For example, the anesthesia coding process includes mapping the CPT code for the surgery with the corresponding anesthesia CPT/ASA codes. This means anesthesia coders must be knowledgeable in anesthesia codes and CPT codes to maintain accuracy.
Anesthesia reimbursement also includes time-based calculations. When multiple anesthesiologists and CRNAs are on the same case, rules for time-based verses unit-based coding can become complex. A well-informed, certified anesthesia coding team will ensure compliance and help you avoid potentially expensive claims issues.
2. Review procedure notes and anesthesia records
Accurate coding requires detailed documentation. Procedure notes and anesthesia records are used to identify the anesthesia start and stop times, the anesthesia technique used, and any anesthesia-related complications that occurred during the procedure.
Creating a checklist for each requirement can help your team easily identify any missing information within the pre-anesthesia evaluation, intraoperative/procedural anesthesia, and post-anesthesia evaluation reports.
3. Code for the correct anesthesia procedure
Anesthesia services can be performed by anesthesiologists, nurse anesthetists, and anesthesiologist assistants. Each practitioner is qualified for a specific range of procedures and payer reimbursements reflect those specialized qualifications.
Coding for the correct anesthesia procedure involves applying the appropriate code for the administrating practitioner so the corresponding reimbursement is accurate. For example, if an anesthesiologist performed general anesthesia and you code for a CRNA instead, you’ll either receive a claim denial or a lower reimbursement.
Plus, each anesthesia procedure has its own specific code. If you know the correct codes for your anesthesia providers and the procedures they perform, you’ll avoid underbilling, overbilling, or resubmitting a claim.
4. Be aware of bundling rules for anesthesia coding
Knowing when your services are meant to be bundled and when they are to be billed separately will help you avoid claim denials, overbilling, and potential compliance issues.
Anesthesia services play a vital role in managing pain, discomfort, and physiological responses during surgical or medical procedures. It is important to note that these services should always be billed separately from the surgical procedure. Anesthesia cannot be included in the procedure billing and therefore must always be submitted as a separate claim.
However, it is worth mentioning that post op pain injections may be bundled into the anesthesia procedure. This is the only instance where bundling rules can apply to the anesthesia billing processes.
5. Know the modifiers and when to use them
Modifiers are two-digit codes appended to a CPT code to provide additional information. In anesthesia coding, modifiers are commonly used to indicate specific circumstances that affect reimbursement. General medical billing software and medical coders unfamiliar with anesthesia-specific requirements often miss this key component of the coding process.
For example, modifiers are used to show medical direction or medical supervision. The modifier “AA” indicates the anesthesia was administered personally by the anesthesiologist. The modifier “QK” indicates the supervising physician medically directed two to four concurrent anesthesia procedures. ¹
If the appropriate modifier is not used, Medicare can reject the claim or reimburse at a lower rate.
Key Takeaways for Anesthesia Coders
Anesthesia coding and payer guidelines are subject to frequent updates. Certified anesthesia coding specialists attend ongoing education and training courses to stay current on the latest trends affecting the anesthesia revenue cycle.
The best way to improve your coding knowledge is to attend workshops, seminars, and webinars. The more you know about documentation and coding practices, the more precise your anesthesia revenue cycle will become.
Are anesthesia coding errors impacting your revenue?
A partnership with a revenue cycle management company specializing in anesthesia can provide you with the right tools and industry knowledge to improve accuracy and compliance.
Find out How an Anesthesia Group Enhanced Cash Flow with nimble’s RCM Expertise in our anesthesia case study.
References:
- Anesthesia Payment Basics Series Codes and Modifiers . (n.d.). Www.asahq.org. https://www.asahq.org/quality-and-practice-management/managing-your-practice/timely-topics-in-payment-and-practice-management/anesthesia-payment-basics-series-codes-and-modifiers
All rights reserved. View our Privacy Policy .

IMAGES
COMMENTS
Assignment 7.8 - Assigning CPT Modifiers. Instructions. Assign the CPT code and appropriate modifier to the following procedural statements. Before assigning the modifier, underline the phrase in each procedure statement that indicates a modifier is to be assigned. (Refer to Table 7-1 of the textbook for assistance in assigning modifiers.)
MODIFIER 91 (repeat clinical diagnostic laboratory test) Reports a laboratory test that was performed on the same day as the original laboratory test. See more. Study with Quizlet and memorize flashcards containing terms like Modifiers, *Appendix A to the CPT Manual*, Modifiers indicate these types of information and more.
When using modifiers such as 25 for a separately identifiable E/M service, it is essential to ensure that the medical record supports the need for the additional service. Proper documentation is key to justifying the use of modifiers and ensuring accurate coding and billing. 7. Use Modifiers Ethically:
STEP 7. Assign the applicable code number and any add-on (+) or additional codes needed to accurately classify the statements. EVALUATION AND MANAGEMENT SYSTEM. (E/M) section (code 99201-99499) is located at the beginning of CPT because these codes describe services most frequently provided by physicians.
The use of modifiers is an important part of coding and billing for health care services. Modifier use has increased as various commercial payers, who in the past did not incorporate modifiers into their reimbursement protocol, recognize and accept HCPCS codes appended with these specialized billing flags.
CH. 9: Exercise 9.8. Assistant surgeon reporting patient's cesarean section, delivery only. Click the card to flip 👆. -80. CPT modifier -80, Assistant Surgeon, is assigned as a functional modifier that impacts the reimbursement paid by the third-party payer. Click the card to flip 👆. 1 / 10.
2.09: CPT Modifiers. When a simple CPT code isn't enough, we turn to CPT modifiers. These important additions to CPT codes give extra information about how, where and why a procedure was performed. This video will introduce and explain CPT modifiers and how to use them. Section 2.01.
Modifiers The Rest of the Story 2 Disclaimer This is not an all inclusive list of every modifier; this is an overview of many modifiers and their intended usage. This material is designed to offer basic information on the use of modifiers in coding. This information is based on the experience, training and interpretation of the author.
2: Medicare will allow payment for assistant at surgery. Append modifier 80, 81, 82, or AS to show that an assistant surgeon was involved in the encounter. 9: Assisted surgery concept doesn't apply. Payers won't reimburse for assistants at surgery in every surgical case, even if you append 80, 81, 82, or AS to the claim.
1. Modifier 21 (Deleted) This modifier was deleted on 01-01-2009 and was used for prolonged evaluation and management services. Instead, you can use CPT 99354, CPT 99355, CPT 99356, CPT 99357, CPT 99358, or CPT 99359. Learn more about the 21 modifier. 2. Modifier 22. Use this modifier for increased procedural services.
CPT ® Modifiers. The modifiers crosswalk is a fast and effective way check allowed modifiers for each CPT ® and HCPCS Level II code. A modifier gives insurers' more information about a claim's procedure or service and often has a financial impact. Omitting or misusing a modifier can cause a claim to be rejected or paid incorrectly.
0. Modifier codes are an important part of medical billing and coding. They provide additional information about a medical procedure or service to help ensure proper reimbursement. Knowing when to use modifier codes can improve claim accuracy and prevent costly payment delays or denials. This comprehensive guide will explain what modifier codes ...
Module 03 Assignment - Apply CPT Coding Guidelines and Modifiers Instructions: Read each scenario and answer the associated questions. Refer to Appendix A and Section coding guidelines in the CPT code book. Be sure to write your answer beneath each question, using complete sentences, reflecting proper spelling and grammar. Scenario 1
A medical coding modifier is two characters (letters or numbers) appended to a CPT ® or HCPCS Level II code. The modifier provides additional information about the medical procedure, service, or supply involved without changing the meaning of the code. Medical coders use modifiers to tell the story of a particular encounter.
• For instance, the appropriate use of -57 can be confusing. While the CPT manual defines this modifier as an E/M service that resulted in the initial decision to perform surgery, Medicare states that it should be used to indicate that the E/M service performed the day before or day of the surgery resulted in the decision for a majorsurgery. 7 8
The 95 modifier is only for codes listed in Appendix P of the CPT manual. Some insurance companies, such as Medicare, accept the 95 modifier. The 95 modifier can be used with a POS of 11 to indicate that the office visit was performed via telehealth. This allows the service to be paid at 100%.
Descriptor. 00790. Anesthesia for intraperitoneal procedures in upper abdomen including laparoscopy; not otherwise specified. 01402. Anesthesia for total knee arthroplasty. As you can observe from these examples, some CPT Anesthesia codes are broad and encompass anesthesia care for a range of diagnostic or therapeutic services (eg, 00790) while ...
Modifiers are two-digit codes appended to a CPT code to provide additional information. In anesthesia coding, modifiers are commonly used to indicate specific circumstances that affect reimbursement. General medical billing software and medical coders unfamiliar with anesthesia-specific requirements often miss this key component of the coding ...